累及后关节面的跟骨骨折需采用手术治疗已经达成共识,传统外侧“L”型扩大入路切口手术后切口并发症较多,随着技术的发展,现已发展出经跗骨窦入路、关节镜辅助复位等技术。 考虑跟骨内松质骨结构,并避免对骨膜及软组织血运造成破坏,有学者创新性采用髓内钉治疗跟骨骨折,并做了系列病例报告,取得良好的治疗效果。

一、Introduction
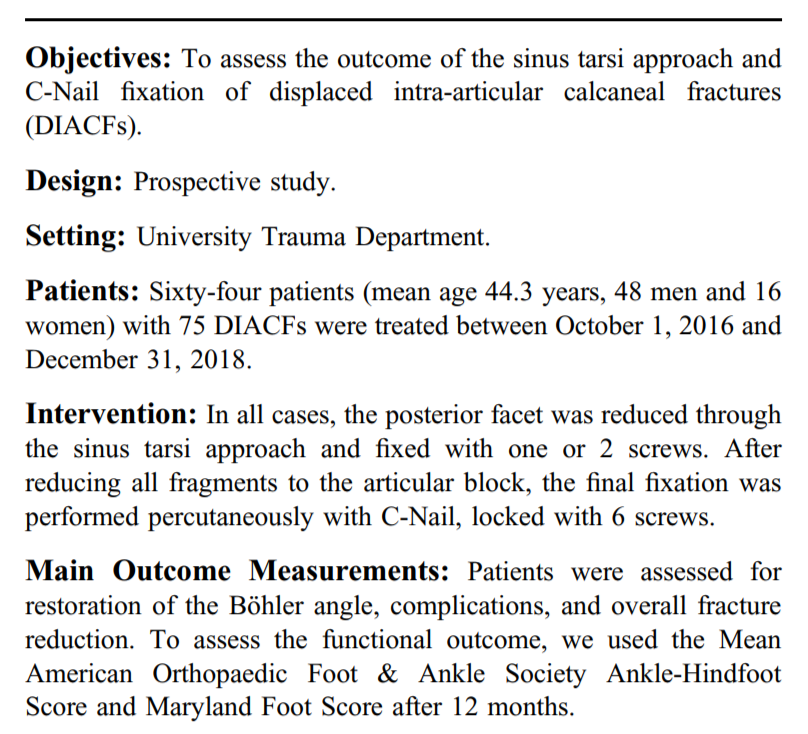
在很长一段时间内,治疗跟骨关节内骨折的金标准是通过扩大外侧入路进行切开复位内固定。然而,这种方法经常与伤口愈合并发症(5.8%-43%)相关,包括血肿、伤口浅表坏死、浅表和深部伤口感染。为了降低这些风险,在过去几年内,微创技术得到了很好的发展,包括经皮螺钉固定、经跗骨窦入路、有限后路和关节镜辅助固定。经跗骨窦入路可直接控制关节复位,无需广泛的软组织解剖,并结合经皮内固定,使软组织并发症发生率较低。在这项研究中,我们旨在评估经跗骨窦入路经皮螺钉固定移位的跟骨关节内骨折的疗效。
techniques were developed over the last several years, including percutaneous screw fixation, the sinus tarsi approach, the limited posterior approach, and arthroscopicassisted fixation. The sinus tarsi approach offers direct control of joint reduction without extensive soft tissue dissection and combined with percutaneous internal fixation, it offers a lower rate of soft-tissue complications. In this study, we aimed to assess the outcome of the sinus tarsi approach using percutaneous nail fixation rather than a plate for the treatment DIACFs. )
二、Objectives
三、Patients
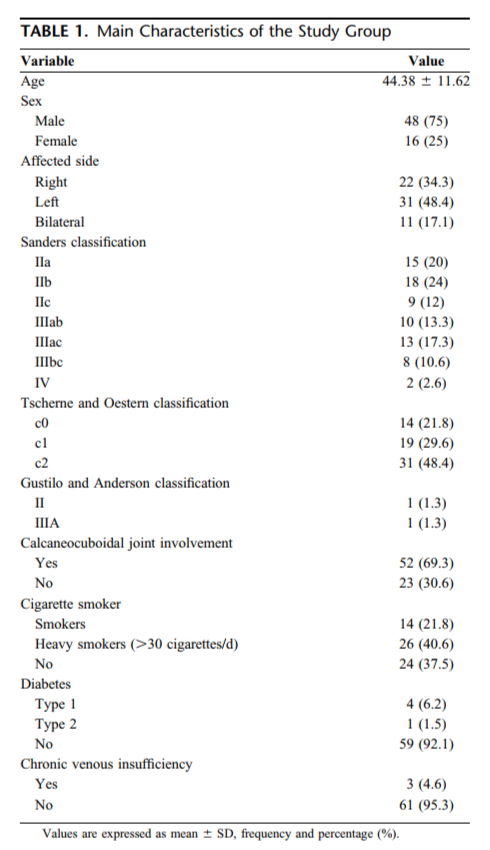
自2016-10-01至2018-12-31,共纳入64例(男48 女16)74足。
(Sixty-four patients (mean age 44.3 years, 48 men and 16 women) with 75 DIACFs were treated between October 1, 2016 and December 31, 2018. )
四、Intervention
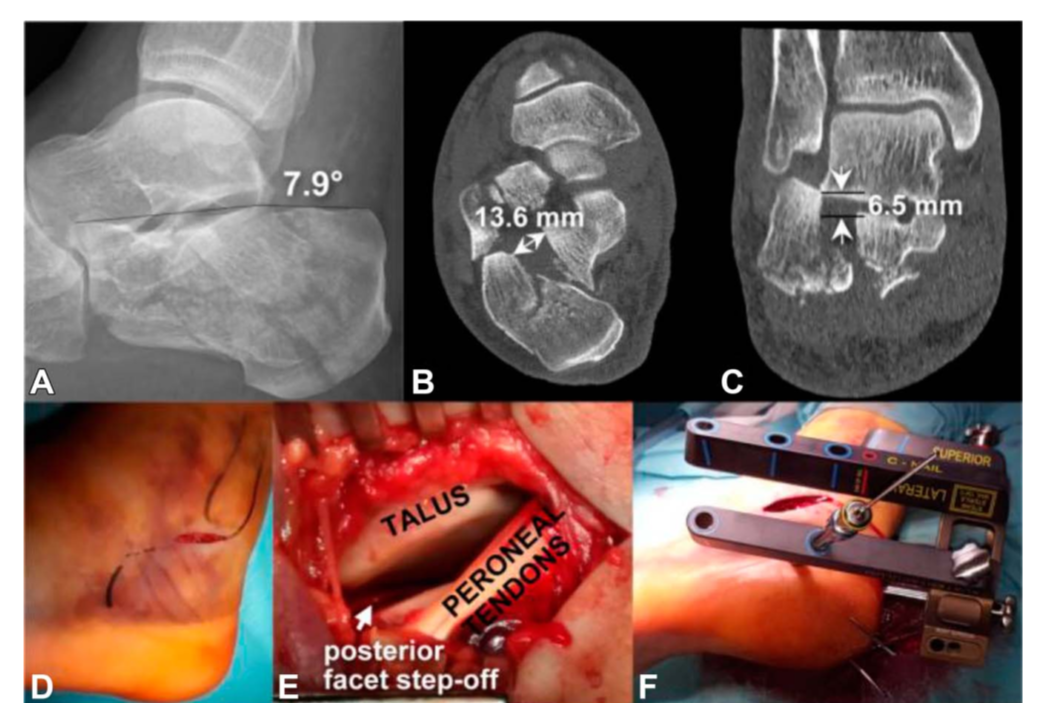
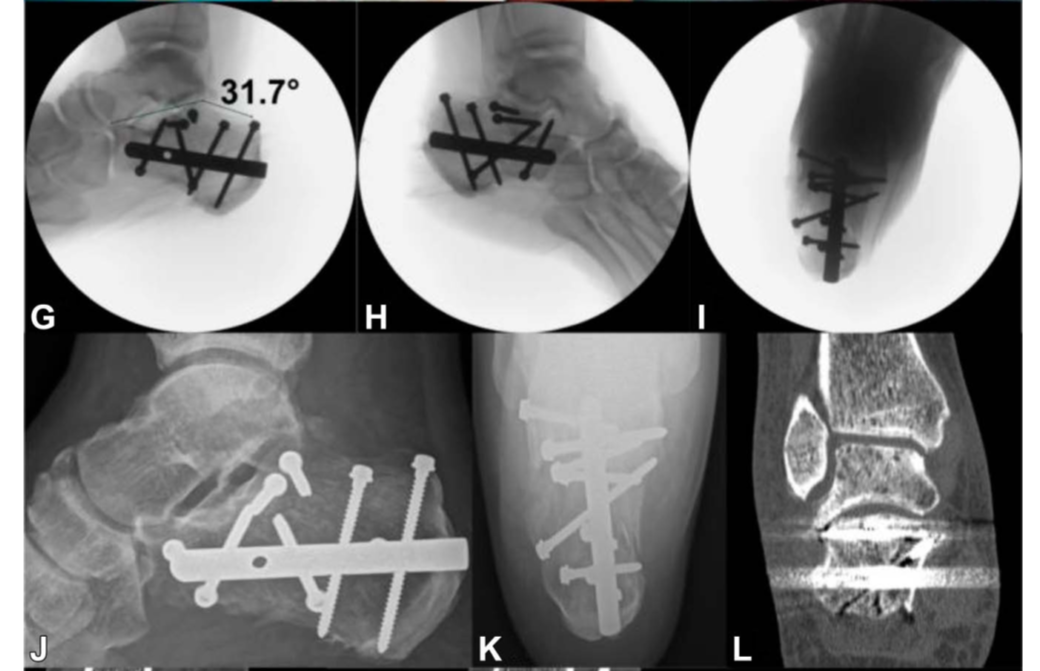
在所有病例中,后关节面通过跗骨窦入路,采用1-2枚螺钉固定。在所有关节的骨块固定后,采用经皮交锁髓内钉固定,6枚锁定钉。

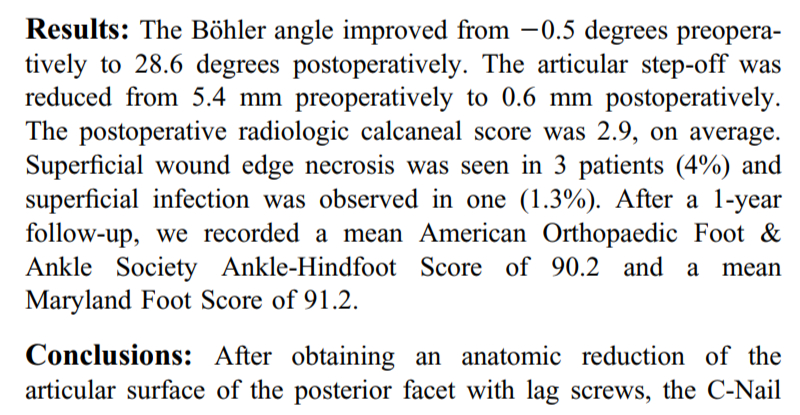
五、Results
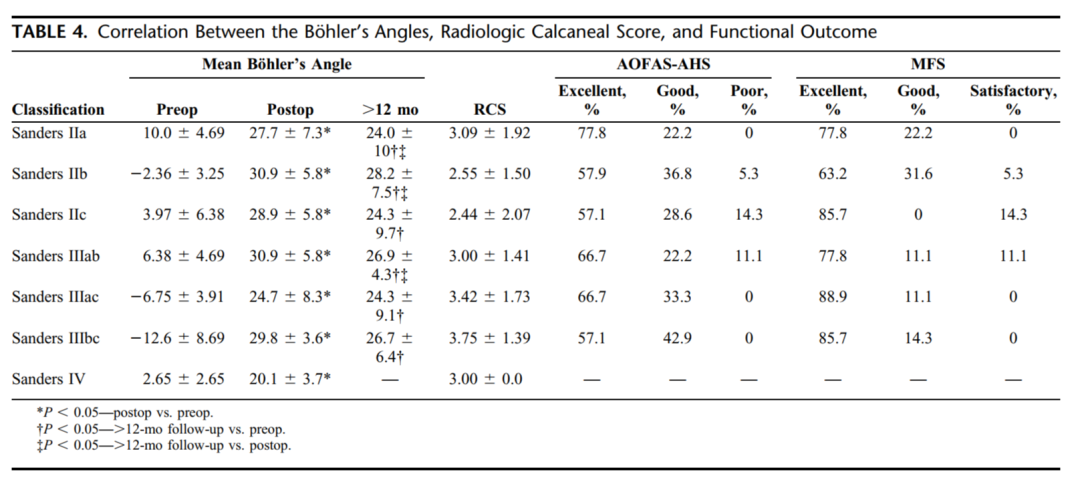
Böhler角由术前的-0.5°纠正到术后28.6°,关节面台阶由术前5.4mm纠正到术后0.6mm,术后影像学评分平均2.9。随后皮肤边缘坏死3例(4%),浅表感染1例(1.3%)。经过1年随访,平均AOFAS评分90.2分,平均Maryland后足评分91.2分。
六、Conclusions
在后关节面通过螺钉获得复位后,交锁髓内钉可以作为移位跟骨关节内骨折具有较好的稳定性和低并发症的一种可选择的方法。
(After obtaining an anatomic reduction of the articular surface of the posterior facet with lag screws, the C-Nail represented a viable alternative to plate stabilization in the treatment of DIACFs, combining primary stability with low soft tissue complications. )

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







感觉手术难度较大
65
学习了
36
#髓内钉#
37
#内固定#
31
#跟骨#
0
学习了,谢谢分享
65