Movement Disorder:复旦·华山医院,PET成像揭示罕见额颞叶痴呆疾病进展
2022-01-15 Freeman MedSci原创 发表于威斯康星
18 F-APN-1607 PET/CT成像对检测MAPT突变携带者的tau积聚有重要意义
额颞叶变性(FTLD)是一个疾病谱,在临床表型、神经病理学特征和遗传基础方面包含了高度异质性的情况。FTLD与tauopathy(FTLD-tau)占所有FTLD病例的40%,微管相关蛋白tau(MAPT)基因的致病突变是FTLD-tau的遗传形式的原因。在生理条件下,产生的具有三个(3R)或四个重复(4R)的微管结合结构域的tau异构体的数量大致相等。
然而,3R和4R tau异构体的相对丰度可被致病的MAPT突变所改变,最终导致3R、4R或3R+4R tauopathies。具体来说,MAPT第10外显子和周围内含子的突变,共同代表了一个重要的热点,这会导致4R tau的过量产生。
最近tau正电子发射断层成像(PET)示踪剂的进展促进了我们识别脑部tau沉积的能力。尽管18F-AV-1451 tau PET已被用于对携带至少10种不同MAPT突变的患者进行成像,但其诊断效果并不一致。尽管该示踪剂与3R+4R tau沉积(主要由MAPT第10外显子以外的突变引起)结合,但对4R tau积累(主要由第10外显子内的突变引起)的可视化能力似乎更为有限。
另一种传统的tau示踪剂11C-PBB3在观察MAPT N279K变体患者的4R tau聚集方面表现良好,但它在临床上受到其固有的代谢不稳定性和快速清除的限制。尽管第二代tau放射性示踪剂18F-PI-2620在进行性核上性麻痹(PSP;一种4R tauopathy)患者中的效用已被调查,但它对MAPT突变携带者是否有临床价值仍未得到解答。
藉此,复旦·华山医院的Xin-Yue Zhou等人,试图通过分析7名具有不同表型的患者样本来研究18F-APN-1607 PET/CT对MAPT突变携带者的临床效用。为此,他们在横断面分析中彻底调查了区域标准化摄取值比(SUVR)和tau沉积的模式。其次,三名患者接受了影像学随访研究,以评估18F-APN-1607 tau PET/CT是否可以作为疾病进展的潜在影像学生物标志物。
他们纳入7名MAPT突变携带者(6名在10号外显子内,1名在10号外显子外)和15名健康对照组。所有参与者在基线时都接受了18F-APN-1607 PET/CT检查。三个10号外显子突变的携带者接受了后续的18 F-APN-1607 PET/CT扫描。
使用小脑灰质作为参考区域,获得了标准化的摄取值比(SUVR)图。在MAPT突变携带者中观察到的SUVR值与健康对照组的数据进行了归一化处理。区域SUVR z-score≥2被用作定义18 F-APN-1607 PET/CT阳性结果的标准。
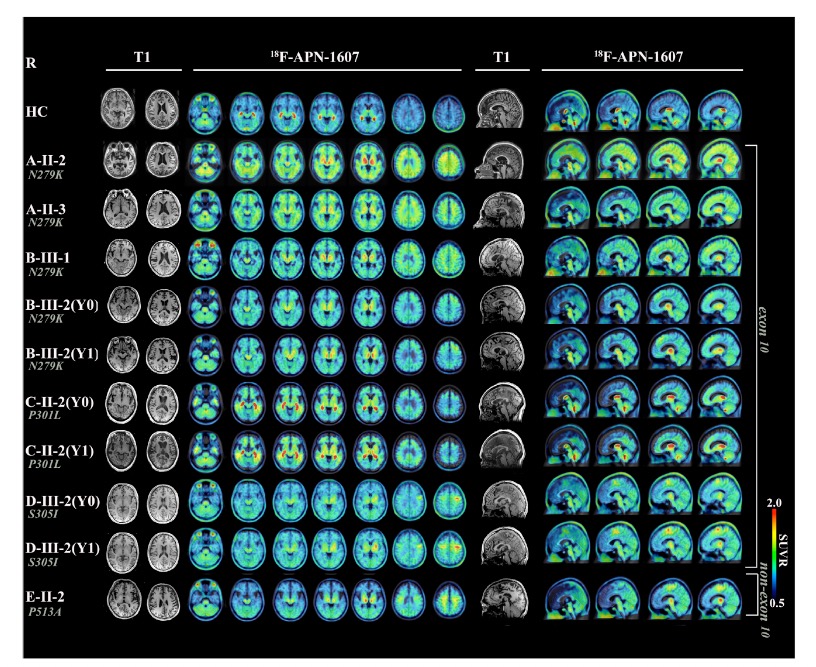
尽管7名研究对象具有不同的临床表型,但所有患者都表现出明显的18 F-APN-1607摄取,其特点是高对比度信号。然而,在具有不同临床症状的患者中,tau沉积的解剖学定位是不同的。三名患者的随访影像资料显示,随着时间的推移,tau积聚的模式有恶化的趋势,这与临床症状的明显恶化相一致。
这个研究的重要意义在于发现了:18 F-APN-1607 PET/CT成像对检测MAPT突变携带者的tau积聚有重要意义。初步随访数据还表明,18 F-APN-1607 PET/CT对监测MAPT突变引起的额颞叶变性的纵向轨迹具有潜在价值。
原文出处:
Zhou X, Lu J, Liu F, et al. In Vivo 18 F‐APN ‐1607 Tau Positron Emission Tomography Imaging in MAPT Mutations: Cross‐Sectional and Longitudinal Findings. Mov Disord. Published online November 29, 2021:mds.28867. doi:10.1002/mds.28867
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#PET成像#
50
#PE#
42
#Disord#
42
#disorder#
46
#Dis#
43
#疾病进展#
25
#PET#
41
#罕见#
47
#复旦#
49
老年性痴呆,未来还是希望借助神经电生理吧,也许更为有效!
28