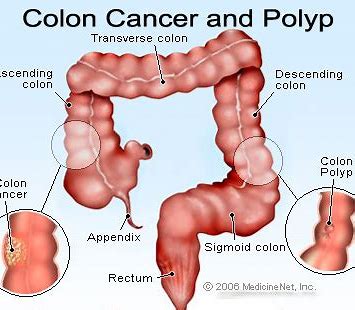
Br J Cancer:错配修复不足的转移性结直肠癌dMMR mCRC患者的生存分析
2020-10-15 xiaozeng MedSci原创
约有5%的转移性结直肠癌(mCRC)患者的肿瘤呈现DNA错配修复不足(dMMR),也称为微卫星不稳定性。dMMR是由于MMR通路发生种系突变、表观遗传甲基化和失活所引起的,导致DNA中的重复序列的插入
约有5%的转移性结直肠癌(mCRC)患者的肿瘤呈现DNA错配修复不足(dMMR),也称为微卫星不稳定性。dMMR是由于MMR通路发生种系突变、表观遗传甲基化和失活所引起的,导致DNA中的重复序列的插入或缺失,基因组超突变和强烈的免疫浸润反应。
既往研究显示,错配修复不足的转移性结直肠癌(dMMR mCRC)患者可从免疫治疗中受益。由于目前全身性非免疫疗法期间的生存数据不足,也使得单臂免疫治疗试验的结果较难分析。
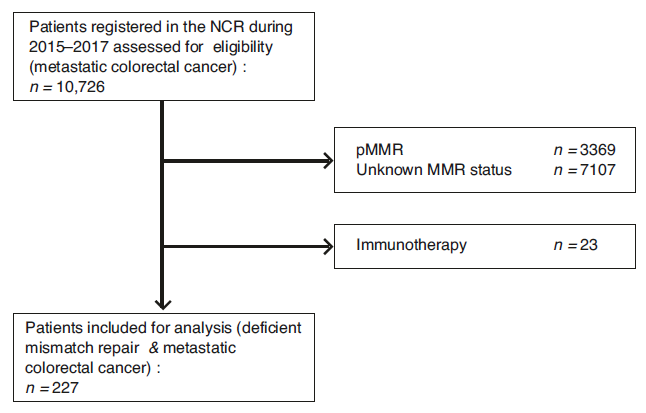
研究流程图
该研究主要提供了使用或不使用系统性非免疫疗法治疗的大量的全面的dMMR mCRC患者队列的生存数据。研究人员一共收集了281例dMMR mCRC患者(54例来自三项前瞻性3期CAIRO试验;227例来自荷兰癌症登记中心)。研究数据分析了确诊mCRC患者在接受一二线全身治疗的总生存期(OS,一二线治疗的总生存期分别用OS1、OS2表示)。并采用Cox回归分析检测相关预后因素。
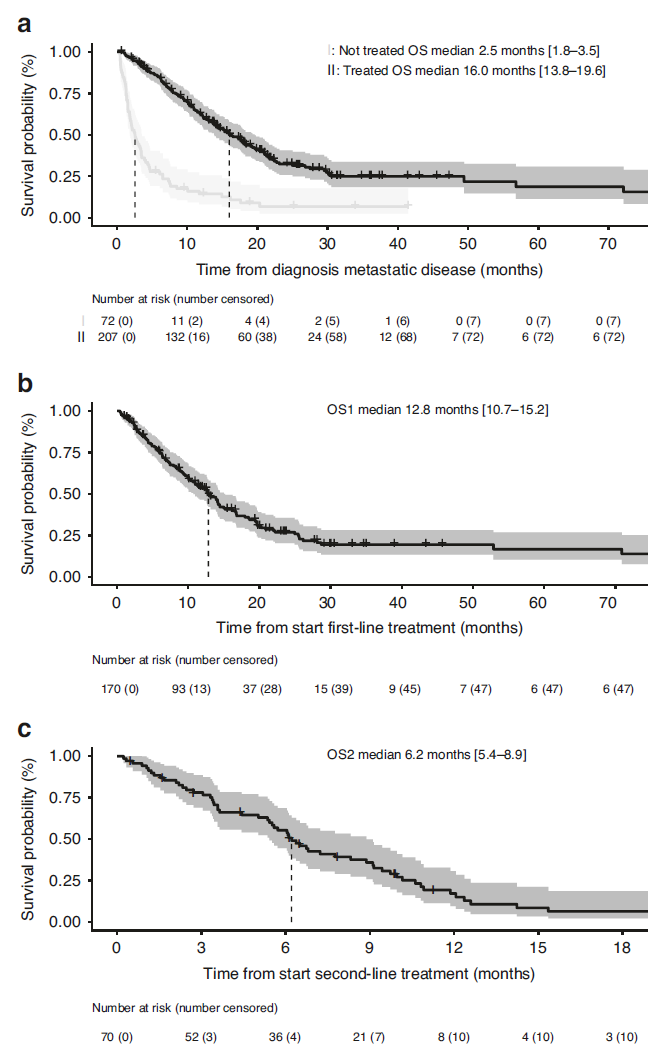
dMMR mCRC患者的总生存期分析
在该研究结果中,281例dMMR患者中,62%的患者接受了一线治疗,26%接受了二线治疗。接受抗肿瘤治疗的OS中位数为16.0个月(13.8-19.6),未接受治疗的患者中位OS为2.5个月(1.8-3.5)。在接受治疗的dMMR患者中,OS1为12.8个月(10.7-15.2),OS2为6.2个月(5.4-8.9)。相比于pMMR患者,接受治疗的dMMR患者的中位OS短了7.6个月。
总而言之,现有的免疫疗法试验的可用数据缺乏标准全身治疗的对照。鉴于与免疫治疗结果相比的一些不良预后,该研究结果强烈暗示了dMMR mCRC患者在免疫治疗过程中的生存获益。
原始出处:
Wensink, G.E., Elferink, M.A.G., May, A.M. et al. Survival of patients with deficient mismatch repair metastatic colorectal cancer in the pre-immunotherapy era. Br J Cancer (13 October 2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#mCRC#
32
#CRC#
37
#转移性#
22
#结直肠#
21
#MMR#
23
学习了
0