近10万患者数据大PK:在防治糖尿病患者的MACE上,三大降糖新药谁最给力?
2022-10-27 MedSci原创 MedSci原创
JAMA Netw Open:恩格列净与利拉鲁肽或西他列汀在不同患者特征的老年人中的疗效比较
与没有T2D的老年人相比,患有2型糖尿病(T2D)的老年人患心血管疾病(CVD)的风险增加。尽管专业协会推荐两类降糖药物,即钠-葡萄糖共转运蛋白2(SGLT2)抑制剂和胰高血糖素样肽-1受体激动剂(GLP-1RA),但在常规护理中采用这些指南仍然是一个挑战,因为有证据表明,它们对心血管的益处在患者亚组中可能并不一致。
但目前,关于恩格列净与替代性二线降糖药物在接受常规治疗且具有广泛心肾风险的T2D患者中的疗效比较的证据依然有限。

因此,本研究比较了恩格列净(近年来使用量不断增加)与(1)利拉鲁肽(最常用的GLP-1RA,已证明心血管益处),和(2)西他列汀(另一种降糖药物类别二肽基肽酶-4 [DPP-4]抑制剂中最常用的药物,已证实对心血管无影响)的相关心血管结局的相关性。
本回顾性研究队列1共纳入45788例患者(22894对倾向评分匹配的恩格列净或利拉鲁肽开始治疗),队列2纳入45624例患者(22 812对倾向评分匹配的用恩格列净或西他列汀开始治疗)。主要结局是(1)改变主要心血管不良事件(MACEs),包括心肌梗死、卒中和全因死亡率的组合,以及(2)心力衰竭住院治疗(HHF)。
结果显示,在队列1的45788例患者中,平均年龄71.9岁(5.1),女性23396例(51.1%),男性22392例(48.9%)。在队列245624例患者中,平均(SD)年龄为72.1(5.1)岁;21418例(46.9%)为女性,24206例(53.1%)为男性。
与利拉鲁肽患者相比,恩格列净患者的MACE结局风险相似 (HR, 0.90;95% CI, 0.79-1.03),而HHF风险降低(HR, 0.66;95% CI,0.52-0.82)。在亚组中,与利拉鲁肽相比,恩格列净与有 ASCVD病史患者的MACE 结局(HR,0.83; 95% CI,0.71-0.98)和 HF(HR,0.77; 95% CI,0.60-1.00)的风险较低相关,并且按性别观察到估计的潜在异质性(男性:HR,0.85 [95% CI, 0.71-1.01];女性:HR,1.16 [95% CI,0.94-1.42]; 同质性P = .02)。然而,在大多数亚组中观察到HHF风险降低(例如,ASCVD:HR,0.66 [95% CI,0.51-0.85];HF:HR,0.66 [95% CI,0.49-0.88])。
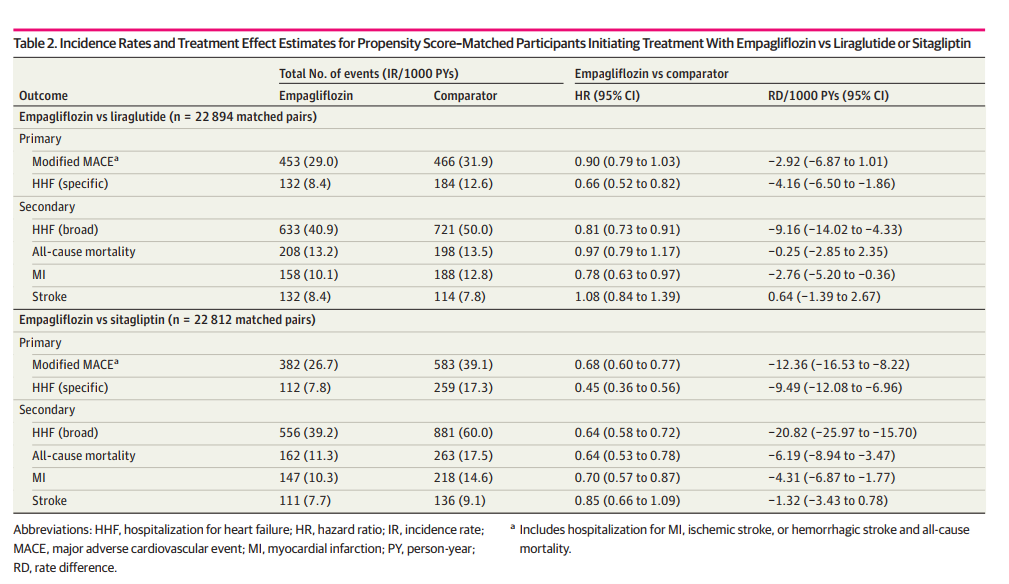
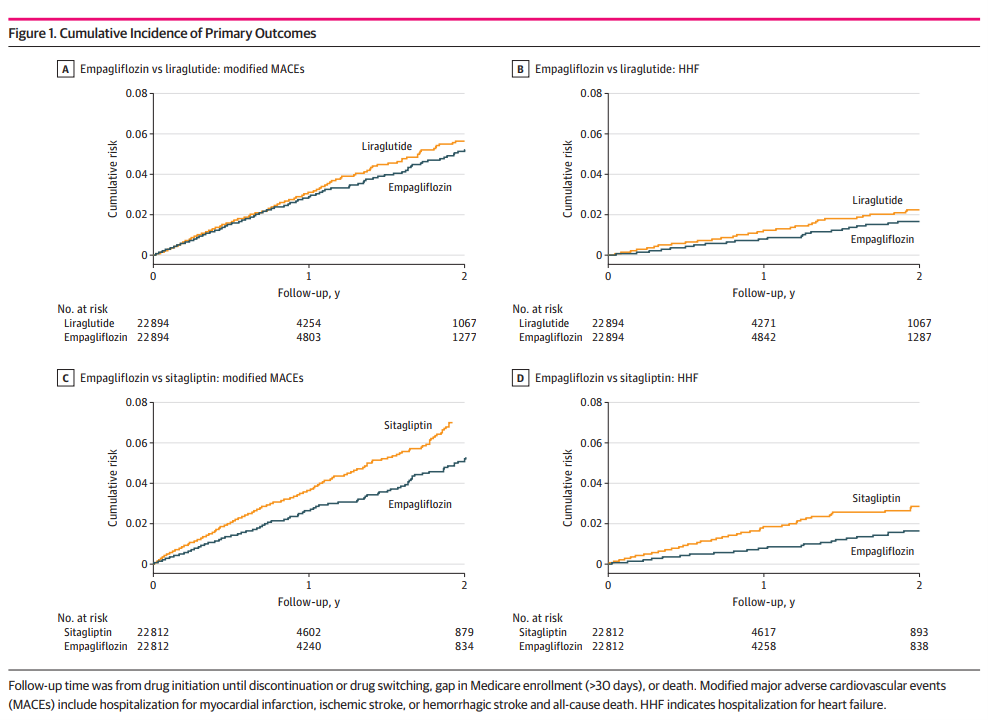
与西他列汀相比,恩格列净与MACE结局(HR,0.68,95%CI,0.60-0.77)和HHF(HR,0.45,95%CI,0.36-0.56)的风险降低相关,这些结果在所有亚组中都是一致的。在有ASCVD病史的患者中,恩格列净相较西他列汀的绝对获益较大(MACE:RD,−17.6 [95% CI,−24.9至-10.4];HHF:RD,−16.7 [95% CI,−21.7 至 −11.9]),HF(MACE: RD, −41.1 [95% CI,−59.9 至 −22.6];HFF:RD,−50.4 [95% CI,−67.5 至 −33.9]),或 CKD(MACE:RD,−26.7 [95% CI,−41.3 至 −12.3];HHF: RD, −31.9 [95% CI, −43.5 至 −20.8])。
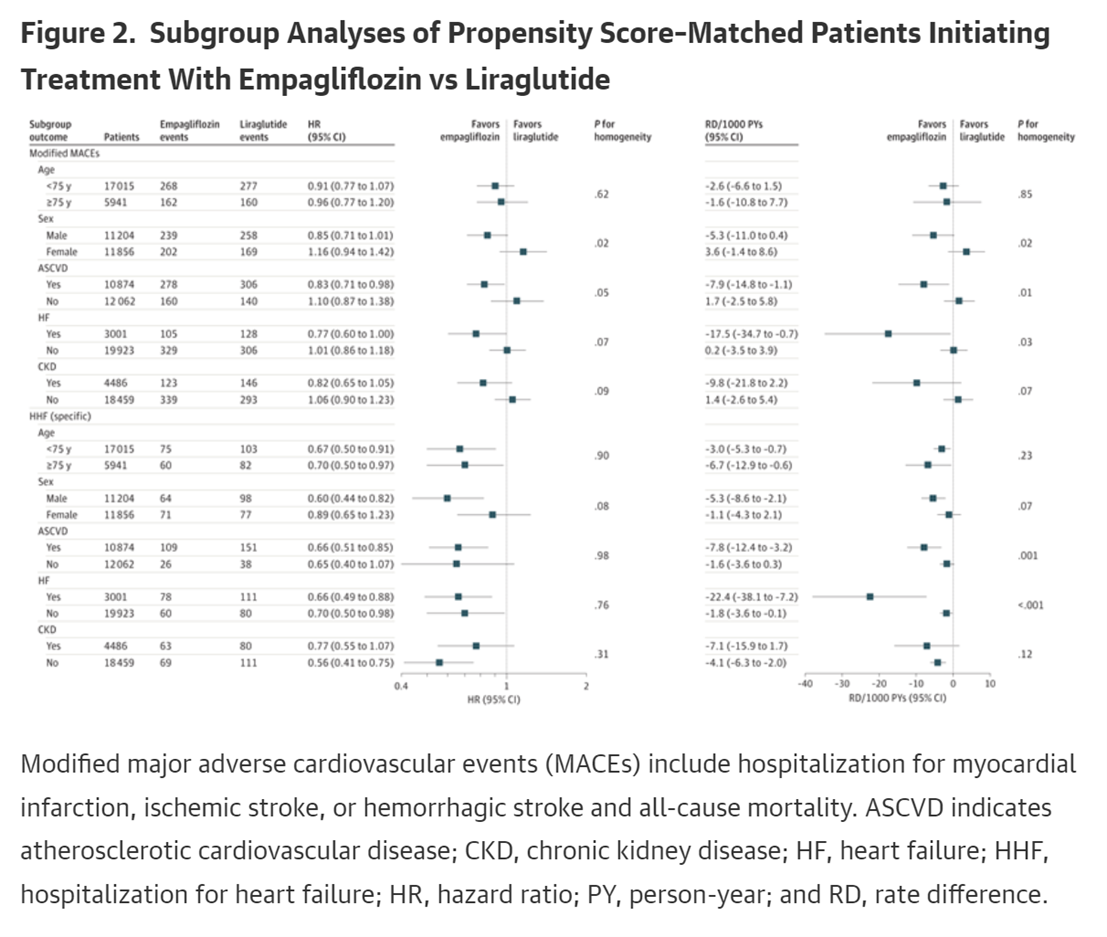
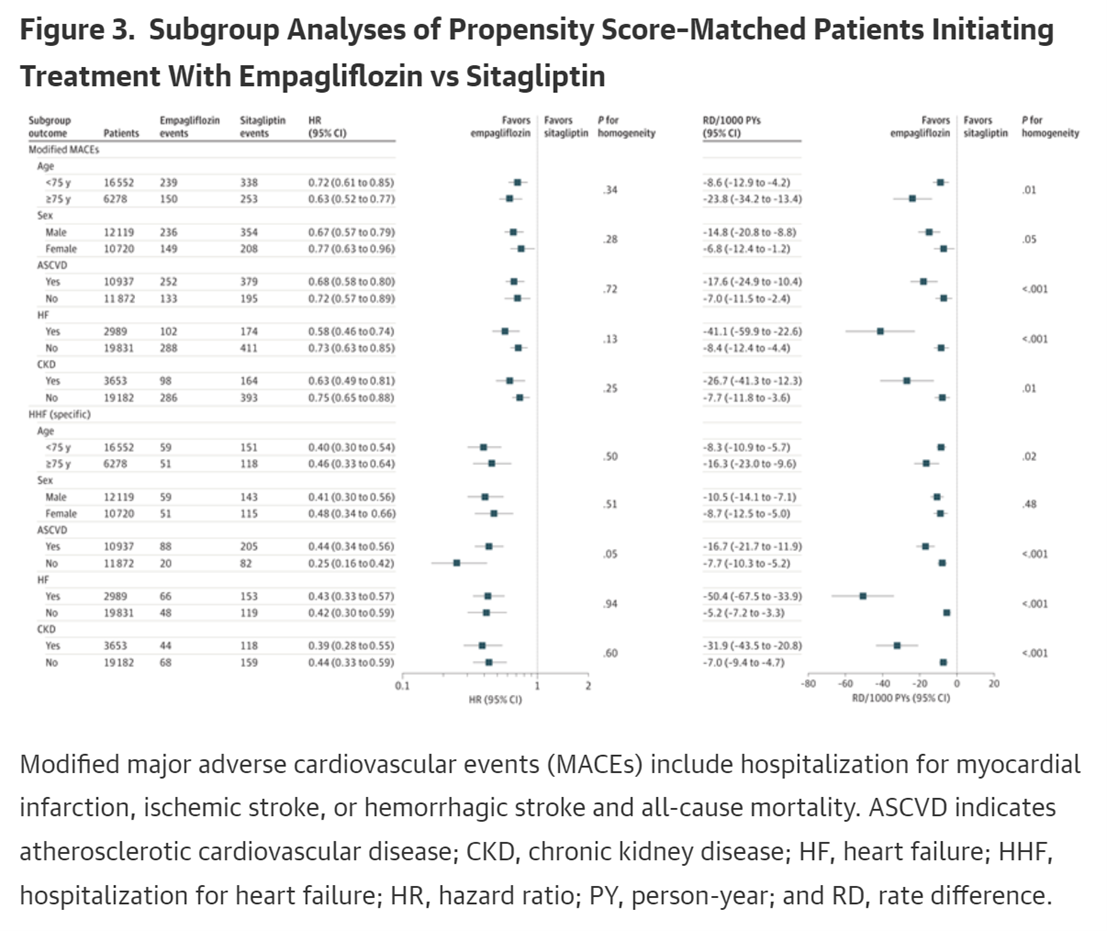
总的来说,在这项针对老年人的疗效比较研究中,恩格列净与较低的HHF (相对于利拉鲁肽和西格列汀)和MACE结果(相对于西格列汀) 风险相关,在确诊的的心肾疾病患者中有较大的绝对收益。这些研究结果表明,与利拉鲁肽或西格列汀相比,老年T2D患者在HHF风险方面可能从恩格列净获益更多;关于MACE的风险,恩格列净可能仅在有心血管疾病史的患者中优于利拉鲁肽,并且在所有患者亚组中优于西他列汀。
原文来源:
Htoo PT, Tesfaye H, Schneeweiss S, et al. Comparative Effectiveness of Empagliflozin vs Liraglutide or Sitagliptin in Older Adults With Diverse Patient Characteristics. JAMA Netw Open. 2022;5(10):e2237606. doi:10.1001/jamanetworkopen.2022.37606
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习了
52
认真学习~
60
学习了,谢谢分享
61
好文章,谢谢分享。
58