JCEM:内源性脱氢表雄酮与女性腰椎骨密度和前臂骨折存在因果关系
2022-01-25 从医路漫漫 MedSci原创
骨质疏松症是一种常见的骨骼疾病,导致骨密度和骨质量降低,增加骨折风险。
背景:骨质疏松症是一种常见的骨骼疾病,导致骨密度和骨质量降低,增加骨折风险。每两个老年妇女中就有一个会在某一时刻患上骨质疏松性骨折。骨折的发生率随着年龄的增长呈指数增长,预计到2050年,全球80岁及以上的人口数量将增加近两倍。
肾上腺源性激素脱氢表雄酮(DHEA)及其硫酸酯(DHEAS)是最丰富的循环类固醇激素。DHEA(S)的许多作用都是通过下游代谢在外周靶组织中转化为具有生物活性的雄激素和雌激素来介导的。肾上腺源性DHEA(S)是绝经前和绝经后女性雄激素的主要来源,也是绝经后女性雌激素的主要来源。循环中的DHEA(S)水平随着年龄的增长而下降,但这种下降背后的机制及其对总体健康的影响尚不清楚。DHEA(S)的年龄相关性下降导致推测DHEA(S)的相对缺乏可能导致常见的年龄相关性疾病的发展,如骨质疏松症。这一观点得到了目前最大的全基因组关联研究(GWAS)血清脱氢表雄酮(DHEAS)荟萃分析结果的支持,该研究表明, 血清脱氢表雄酮(DHEAS)的遗传决定因素与衰老的生物学途径有关
最近一项对四个临床试验的综合分析表明,脱氢表雄酮(DHEA)治疗可增加女性腰椎骨密度(LS-BMD)。内源性肾上腺衍生脱氢表雄酮硫酸盐(DHEAS)对女性LS-BMD和骨折风险的因果影响尚不清楚。
目的:确定循环DHEAS与女性腰椎骨密度(LS-BMD)和骨折风险是否存在因果关系。
方法:一项双样本孟德尔随机研究,使用血清DHEAs的遗传预测因子,使用现有最大的女性特异性基因组广泛关联研究(GWAS)荟萃分析(n=8565)。基因与DXA衍生的骨密度(n=22900)的关联来自GEFOS联盟提供的女性特定的GWAS汇总统计数据,而来自英国生物库的238565名白人血统妇女的个体水平数据用于评估骨折(前臂骨折11564例,髋部骨折2604例)的关系,并通过超声波估计足跟骨密度(EBMD)。
结果:1标准差(SD)的对数血清DHEAS水平增加与LS骨密度增加0.21SD(P值:0.01)和eBMD0.08SD增加(P值:<0.001)相关。基因预测的DHEAS降低了前臂骨折的风险(优势比(OR):0.70,95%可信区间(CI):0.55-0.88),而与髋部骨折没有明显的因果关系。

图1 估计DHEAS对女性腰椎骨密度(LS-BMD)和股骨颈骨密度(FN-BMD)的因果影响。
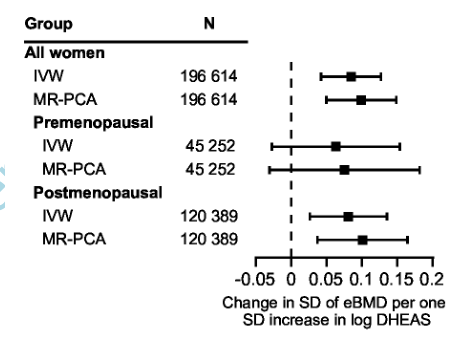
图2 DHEAS对女性足跟超声估计BMD (eBMD)的因果影响。

图3 DHEAS对女性骨折风险的因果影响估计。
结论:基因预测的血清DHEAS增加女性LS-BMD,降低前臂骨折风险。根据目前的研究结果和以前的脱氢表雄酮治疗随机对照试验,我们认为内源性肾上腺来源的脱氢表雄酮(S)和脱氢表雄酮的药物治疗都能改善女性的骨健康。
原文出处:Quester J, Nethander M, Eriksson A,et al.Endogenous DHEAS is Causally Linked with Lumbar Spine Bone Mineral Density and Forearm Fractures in Women.J Clin Endocrinol Metab 2021 Dec 22
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JCEM#
38
#腰椎骨#
53
#内源性#
37
#JCE#
34
#腰椎#
45