Clin Rheumatol:日常临床实践中戈利木单抗治疗RA、AS和PsA的治疗持续性
2018-12-27 Rheum情报官 Rheum情报官
与其他TNFi相比,日常临床实践中戈利木单抗治疗RA、AS和PsA的治疗持续性:一项来自斯洛文尼亚的患者使用bDMARDs治疗的全国性、纵向、观察性登记研究—BioRx.si Rotar Ž等研究者于2018年10月15日在Clinical Rheumatology上在线发表一项研究,旨在评估戈利木单抗(GLM)与其他肿瘤坏死因子-α抑制剂(TNFi)治疗斯洛文尼亚类风湿关节炎(RA
与其他TNFi相比,日常临床实践中戈利木单抗治疗RA、AS和PsA的治疗持续性:一项来自斯洛文尼亚的患者使用bDMARDs治疗的全国性、纵向、观察性登记研究—BioRx.si
Rotar Ž等研究者于2018年10月15日在Clinical Rheumatology上在线发表一项研究,旨在评估戈利木单抗(GLM)与其他肿瘤坏死因子-α抑制剂(TNFi)治疗斯洛文尼亚类风湿关节炎(RA)、强直性脊柱炎(AS)和银屑病关节炎(PsA)患者的持续性。
GLM是治疗RA、AS和PsA的肿瘤坏死因子-α抑制剂(TNFi)之一。GLM与其他TNFi疗效和安全性相当,且在皮下注射TNFis中具有给药间隔最长的优势。TNFi在临床试验内的效度稳健。然而,由于严格的纳入和排除标准,日常临床实践中接受治疗的患者仅有不到10%被纳入临床试验。目前已经建立了纵向观察性研究来评估临床试验结果的外部效度。由于研究设计的性质,这些研究会在一些地方受到挑战,如随访时间点不规则、数据不完整和偏差,经常数据分析及结果解释。而在这种情况下,评估治疗有效性和耐受性的替代指标——治疗持续性则比较简单。
该研究针对2010年1月1日至2018年7月31日从强制性国家BioRx.si登记处收集的所有使用GLM和其他TNFi治疗患者的数据,进行了前瞻性分析。采用Kaplan-Meier方法和已校正公认混杂因素的Cox比例回归风险模型,根据治疗类型、适应症和之前暴露于生物缓解病情抗风湿药(bDMARDs)分层来评估治疗持续性。并评估了其在治疗开始后1年时的有效性。
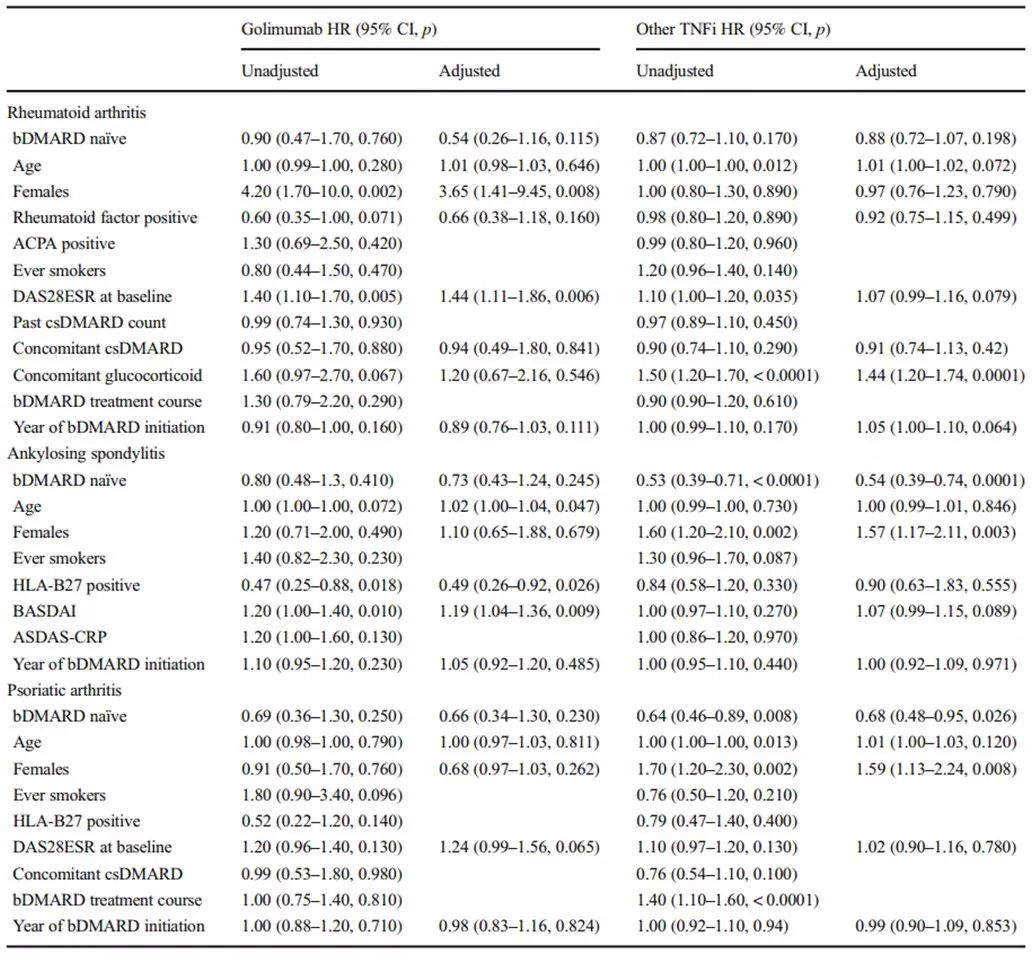
在7年观察期间,来自8个中心的24名斯洛文尼亚风湿科医师分别提供了使用GLM治疗的368例患者和使用其他TNFi治疗的1654例患者的849人-年和3321人-年的数据。开始治疗后2年时仍接受GLM与其他TNFi治疗的RA、AS和PsA患者总比例无显著差异,分别为53% vs. 47%、67% vs. 65% 和59% vs. 59%。对于RA、AS和PsA,既往未使用过bDMARD和bDMARD暴露患者中发生GLM停药的粗、校正后危险比无显著差异(图1)。此外,在既往未使用过bDMARD和bDMARD暴露的RA患者中,GLM和其他TNFi组的粗、校正治疗持续率相当(表1)。在既往未使用过bDMARD和bDMARD暴露的AS和PsA患者中,GLM组粗、校正治疗持续率相当,而其他TNFi组bDMARD暴露患者的粗、校正治疗持续率则显著降低(表1)。斯洛文尼亚RA、AS和PsA患者的GLM治疗持续性与更富裕的西欧国家相当。
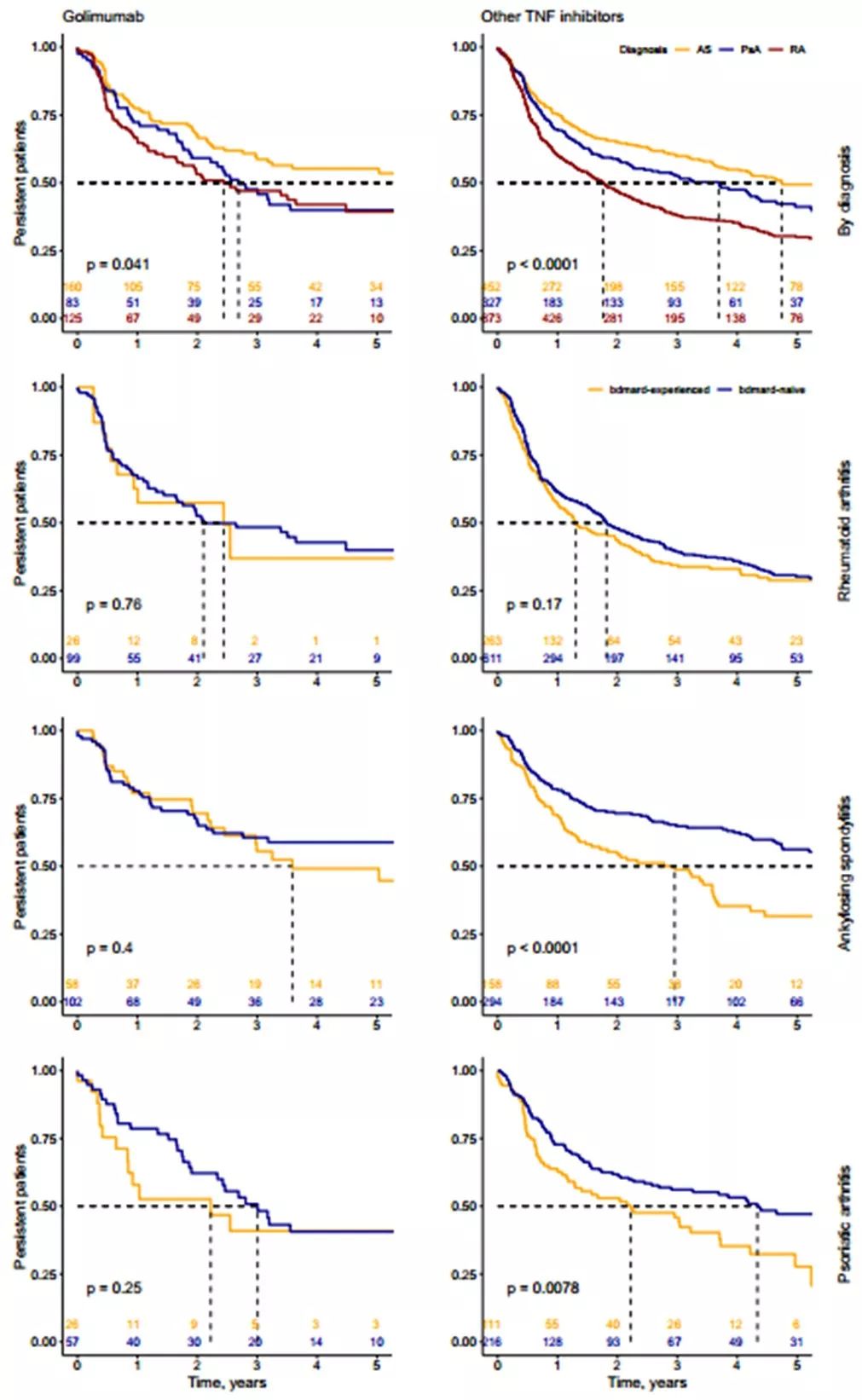
图1. 基于适应症以及基于适应症和bDMARDs既往暴露情况的戈利木单抗治疗持续性
表1. 基于既往bDMARD暴露情况,针对GLM和其他TNFi治疗持续性的单变量和多变量Cox 比例风险模型
针对从斯洛文尼亚国家强制性在线登记处收集的bDMARDs治疗患者的前瞻性数据进行的分析(BioRx.si),是探讨和比较GLM与其他TNFi治疗持续性和有效性的少数真实世界研究之一,也是观察期(7年)最长的研究之一,并显示GLM的治疗持续性与其他TNFis以及来自其他真实世界的观察报告结果相当。此外,斯洛文尼亚数据集也表明,在所研究的任何风湿适应症中,既往bDMARD暴露对GLM的治疗持续性无显著影响,但在2010年1月1日之后开始TNFi治疗的bDMARD经治AS和PsA患者中,其他TNFis的治疗持续性较低。此外,这也是针对代表性不足的中欧地区受试者的首项报告。
总之,GLM治疗斯洛文尼亚RA、AS和PsA患者的持续性与更富裕的西欧国家相当。对所有研究的适应症而言,GLM和其他TNFi的总体治疗持续性也相当。值得注意的是,该研究观察到无论针对哪个适应症,GLM用于既往未使用过bDMARD和bDMARD暴露患者的治疗持续性无差异,但在既往bDMARD暴露的AS和PsA患者中,其他TNFi的治疗持续性显著降低。这也提示在既往bDMARD暴露的AS和PsA患者中,GLM较其他TNFi具有更好的治疗持续性。
原始出处:
Rotar Ž, Tomšič M, Praprotnik S, et al. The persistence of golimumab compared to other tumour necrosis factor-α inhibitors in daily clinical practice for the treatment of rheumatoid arthritis, ankylosing spondylitis and psoriatic arthritis: observations from the Slovenian nation-wide longitudinal registry of patients treated with biologic disease-modifying antirheumatic drugs-BioRx.si.Clin Rheumatol. 2018 Oct 15.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#持续性#
29
#PSA#
30
#临床实践#
30
#戈利木单抗#
46
学习谢谢分享
71