Eur Urol:前列腺根治性切除术候选患者的一种新型风险分层方法
2021-08-26 AlexYang MedSci原创
目前,前列腺癌(PCa)患者在前列腺根治术(RP)治疗后,生化复发(BCR)的风险分类系统仍然只基于临床变量,并没有考虑磁共振成像(MRI)参数。
目前,前列腺癌(PCa)患者在前列腺根治术(RP)治疗后,生化复发(BCR)的风险分类系统仍然只基于临床变量,并没有考虑磁共振成像(MRI)参数。

近期,意大利研究人员在《Eur urol》杂志上发表文章,开发和验证了一种整合了临床和放射学参数的新型分类系统。

在2014年至2020年期间,研究人员在七个国际转诊中心进行了一项回顾性多中心队列研究,包括2565名接受RP治疗的PCa患者。
BCR定义为RP后3年内出现两次前列腺特异性抗原(PSA)值≥0.2 ng/ml。Kaplan-Meier和Cox回归测试了BCR的发生时间和预测因素。开发和验证队列由整个患者样本产生。预测因素包括PSA、活检等级组、MRI阶段和病变的最大直径。之后,使用Harrel's一致性指数(c-index)比较了新型风险分层系统与欧洲泌尿外科协会(EAU)、前列腺癌风险评估(CAPRA)和国际前列腺癌分期合作组织(STAR-CAP)风险组在预测早期BCR方面的准确性。
根据EAU风险组,分别有200人(8%)、1834人(71%)和531人(21%)为低、中、高风险。3年总体无BCR生存率为84%。EAU低风险组和中风险组之间的3年无BCR生存率没有差异(88% vs 87%;P=0.1)。新型列线图在外部验证时表现出了最佳的分辨力(c-index 78%)。根据基于Cox列线图中的预测因素,确定了四个新的风险类别。新的风险分类在预测早期BCR方面的准确率(c-index 70%)高于EAU、CAPRA和STAR-CAP风险分类(c-index分别为64%、63%和67%)。
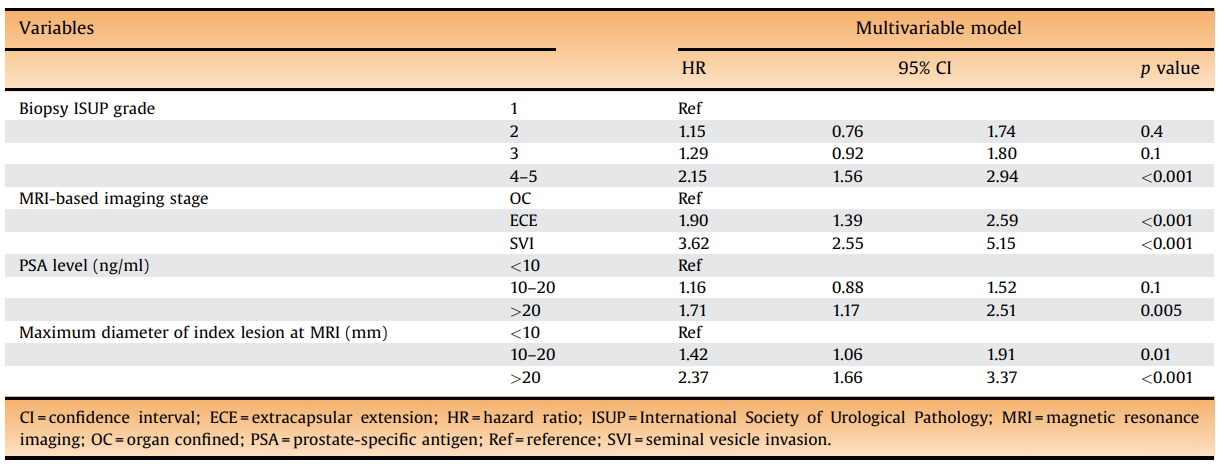
整合了放射学和临床参数的多变量Cox回归分析预测术后生化复发结果情况
综上所述,根据临床和放射学参数开发并外部验证的这四种新的分类,可有效预测早期BCR。这种新型分类法比现有工具有更高的准确性。
原始出处:
Elio Mazzone , Giorgio Gandaglia , Guillame Ploussard et al. Risk Stratification of Patients Candidate to Radical Prostatectomy Based on Clinical and Multiparametric Magnetic Resonance Imaging Parameters: Development and External Validation of Novel Risk Groups. Eur Urol. Aug 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#切除术#
42
#风险分层#
45
#根治性切除术#
38
#根治#
27
哦卡嗯啦
59
很棒
62