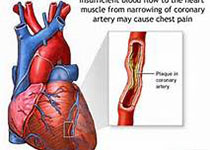
JACC:口服氟喹诺酮药物会增加主动脉和二尖瓣反流风险
2019-09-15 不详 MedSci原创
近期有研究认为氟喹诺酮类药物(FQs)与心脏不良事件的发生相关,包括主动脉夹层和动脉瘤。截止目前,FQs是否会增加主动脉或二尖瓣反流风险尚不清楚。本研究的目的旨在评估FQs是否会增加主动脉或二尖瓣反流风险。本研究纳入了美国IQVIA数据库中的12505名患者和125020名对照,与阿莫西林和阿奇霉素的使用者相比,FQs使用者发生主动脉或二尖瓣反流风险的比值比(RR)为 2.40 (95% CI:
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#喹诺酮#
36
#JACC#
0
#ACC#
33
#主动脉#
31
#二尖瓣#
30
#氟喹诺酮#
0
#反流#
23