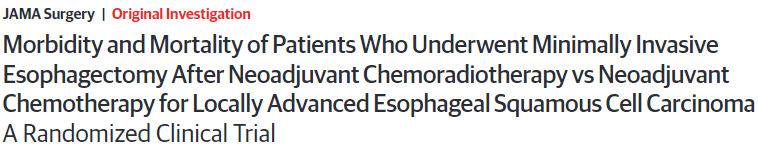
JAMA Surg:局部晚期食管癌食管切除术前是新辅助放化疗还是新辅助化疗?
2021-03-19 Nebula MedSci原创
局部晚期食管癌患者采用单纯手术治疗往往会复发或转移,导致患者预后不良,术前是额外予以新辅助放化疗还是新辅助化疗?
食管癌是全球常见的一种癌症。食管癌切除术仍是当下食管癌治疗的基石。但局部晚期食管癌患者采用单纯手术治疗往往会复发或转移,导致患者预后不良。因此,多学科治疗被强力推荐以改善这类患者的预后。
由于缺乏高水平的临床证据,新辅助放化疗(nCRT)对比新辅助化疗(nCT)治疗局部晚期食管鳞癌(ESCC)的安全性和有效性仍不确定。
本研究旨在比较微创食管切除术(MIE)前予以nCRT或nCT治疗局部晚期ESCC的安全性和远期生存率。
这是一项前瞻性、多中心、开放标签的随机临床试验,纳入了264例临床分期为cT3~T4aN0~1M0的ESCC患者,随机分为nCRT组(n=132)或nCT组(n=132)。两组均予以以紫杉醇和顺铂为基础的化疗,nCRT组加用40Gy同步放疗。在新辅助治疗后6周左右,两组患者均在胸腔镜和腹腔镜联合下进行MIE。主要结果是3年总生存期。次要结果包括术后并发症、死亡率、术后病理结果、无复发生存时间和生活质量。
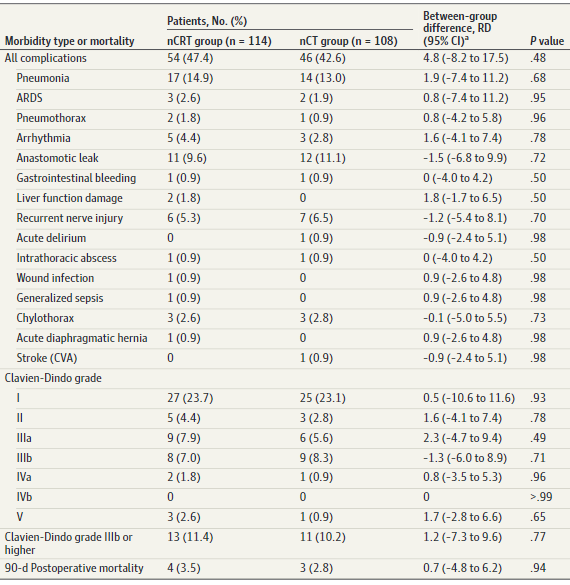
手术预后
在264例患者(男性226例,占85.6%;平均 61.4岁)中,nCRT组的术后发病率为47.4%(54/114),而nCT组的为42.6%(46/108),两组间差异无显著性意义(差异 4.8%;95%CI -8.2%~17.5%;P=0.48)。
发病率和死亡率
根据Clavien-Dindo分类,两组患者的并发症严重程度分布相似。围手术期死亡率:nCRT组为3.5%(4/114),nCT组为2.8%(3/108)(P=0.94)。两组间R0切除率相近(109/112[97.3%] vs 100/104[96.2%];P=0.92)。
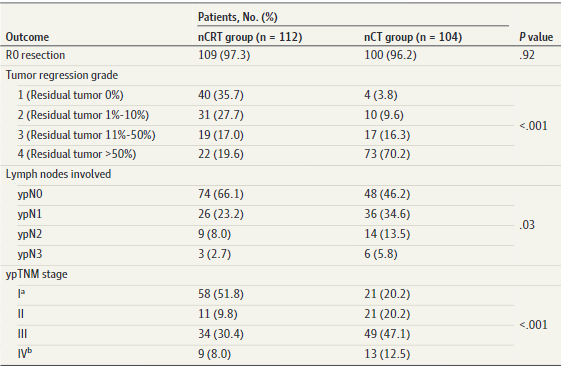
病理预后
但是,nCRT组的病理完全缓解率(残留肿瘤 0%)明显高于nCT组(40/112[35.7%] vs 4/104[3.8%];P<0.001),淋巴结转阴率明显高于nCT组(ypN0,74/112[66.2%] vs 48/104[46.2%];P=0.03)。
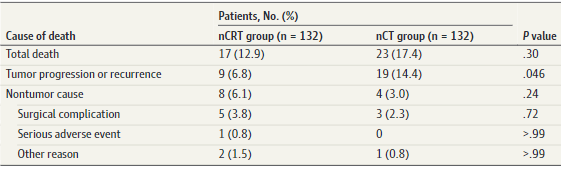
一年内死因
在意向处理分析中,nCRT组一年总生存率为87.1%(115/132),而nCT组的为82.6%(109/132)(P=0.30)。此外,nCRT组肿瘤进展或复发导致的死亡明显低于nCT组(9/132[6.8%] vs 19/132[14.4%];P=0.046);但是,两组的非肿瘤原因死亡相近(8/132[6.1%] vs 4/132[3.0%];P=0.24)。
总之,本试验的初步结果显示,对于局部晚期食管鳞癌,nCRT+MIE与nCT+MIE相比,具有相似的安全性和更好的组织病理结局。
原始出处:
Wang Hao,Tang Han,Fang Yong et al. Morbidity and Mortality of Patients Who Underwent Minimally Invasive Esophagectomy After Neoadjuvant Chemoradiotherapy vs Neoadjuvant Chemotherapy for Locally Advanced Esophageal Squamous Cell Carcinoma: A Randomized Clinical Trial. JAMA Surg, 2021, 10.1001/jamasurg.2021.0133
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#切除术#
35
#新辅助#
37
#食管切除术#
31
#局部晚期#
26
学习了
59
#辅助放化疗#
29
#放化疗#
22
#局部#
31
#新辅助放化疗#
29
#食管#
30