ARD: 羟氯喹减少或停药后的发作:系统性狼疮国际合作诊所 (SLICC) 初始队列的结果
2022-05-17 MedSci原创 MedSci原创
HCQ减量/停药后SLE发作风险高于HCQ维持。维持、减少或停止HCQ的决定可能会对特定亚组产生不同的影响,包括使用泼尼松和/或教育程度低的亚组。
目的:在临床实践中,患者经常向医生咨询羟氯喹 (HCQ) 减量或停药。文献和临床经验表明在一些稳定的患者中HCQ减量/停药可能是安全的,但在其他情况下可能与疾病发作有关。本研究目的在于评估羟氯喹(HCQ)减少或停药与HCQ维持用药的系统性红斑狼疮 (SLE) 发作情况。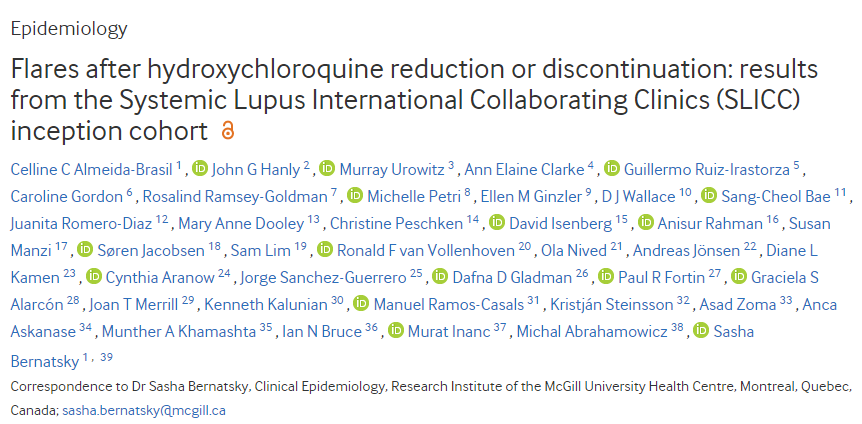
方法:该研究团队分析了系统性狼疮国际合作诊所 (SLICC) 队列的前瞻性数据,该队列在SLE诊断后15个月内从33个地点入组,并每年进行一次随访(1999-2019 年)。研究者评估了初始HCQ剂量(“维持”)时的人时贡献,并将其与第一次剂量减少后和第一次HCQ停药后的人时进行比较。研究人员估计了第一次SLE发作的时间,发作定义为随后需要加强治疗、SLE 疾病活动指数-2000增加≥4点或因SLE住院。估计了调整后的HR (aHR),其中95%CI与减少/停止使用HCQ相关(相对于维持HCQ)。研究人员还在每个 HCQ子队列中进行了单独的多变量风险回归,以确定与SLE发作相关的因素。
结果:研究了1460名(90% 女性)开始使用HCQ的患者。HCQ减少组和停药组与HCQ 维持组相比,首次SLE发作的aHR分别为1.20(95% CI 1.04 -1.38)和1.56(95% CI 1.31 -1.86)。受教育程度低的患者在停用HCQ后更容易发作(aHR 1.43,95% CI 1.09-1.87)。在所有HCQ亚队列中,在零时间使用泼尼松与超过1.5倍的发作风险增加相关。
结论:HCQ减量/停药后SLE发作风险高于HCQ维持。维持、减少或停止HCQ的决定可能会对特定亚组产生不同的影响,包括使用泼尼松和/或教育程度低的亚组。对特殊群体(例如老年人)的进一步研究可能会有所帮助。
出处:
Almeida-Brasil CC, Hanly JG, Urowitz M, et al. Flares after hydroxychloroquine reduction or discontinuation: results from the Systemic Lupus International Collaborating Clinics (SLICC) inception cohort. Annals of the Rheumatic Diseases Published Online First: 15 December 2021. doi: 10.1136/annrheumdis-2021-221295
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#系统性#
54
#SLICC#
59
#国际合作#
44
疾病竟然和教育程度有关?
59
好东西,谢谢分享
56
#诊所#
30
#狼疮#
35
#停药#
39
#ICC#
33