Intens Care Med:铜绿假单胞菌呼吸机相关性肺炎长期和短期抗生素治疗比较
2022-05-23 MedSci原创 MedSci原创
短期和长期抗生素治疗铜绿假单胞菌-呼吸机相关性肺炎的复合或单独结局(90天死亡率或呼吸机相关性肺炎复发)没有差异。
与长时间的抗生素治疗相比,短程抗生素治疗的呼吸机相关性肺炎的临床疗效相当。近日,危重病医学领域权威杂志Intensive Care Medicine上发表了一篇研究文章,研究人员的目的是评估短期抗生素治疗(8天)与长期抗生素治疗(15天)在因铜绿假单胞菌引起的呼吸机相关性肺炎(铜绿假单胞菌-呼吸机相关性肺炎)疗效中的非劣效性。
研究人员开展了一项全国性、随机、开放标记、多中心、非劣效性试验,以评估铜绿假单胞菌-呼吸机相关性肺炎患者接受抗生素治疗的最佳持续治疗时间。符合条件的患者是诊断为铜绿假单胞菌-呼吸机相关性肺炎的成年患者,他们按1:1的比例随机分配接受短期(8天)或长期(15天)抗生素治疗。研究人员使用预先指定的分析来评估在重症监护病房(ICU)住院90天内的死亡率和铜绿假单胞菌-呼吸机相关性肺炎复发率的复合结局。

在意向治疗人群(n=186)中,15天治疗组达到复合结局患者的百分比为25.5%(n=25/98),而8天治疗组达到复合结局患者的百分比为35.2%(n=31/88)(差异为9.7%,90%置信区间(CI)为0-21.2%)。
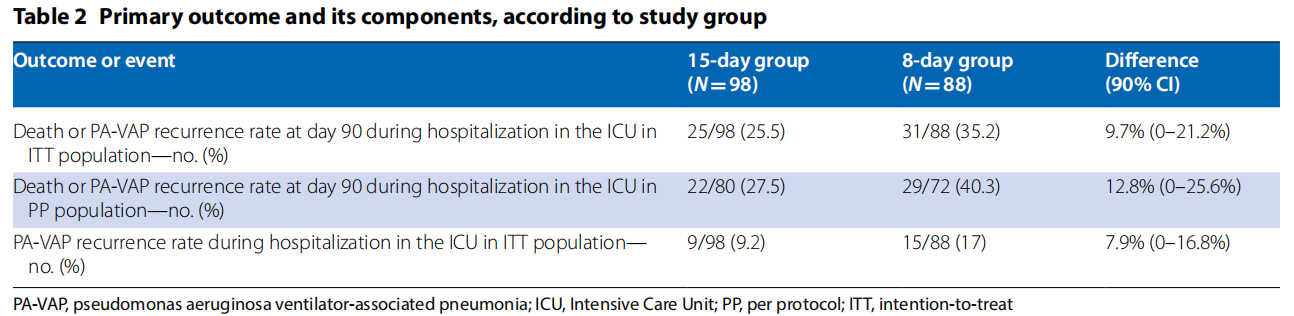
ICU住院期间15天治疗组铜绿假单胞菌-呼吸机相关性肺炎复发率为9.2%,8天治疗组为17%。两组患者在ICU期间机械通气天数、ICU住院天数、肺部感染和多重耐药病原体获得的中位天数相似。
由此可见,该研究结果显示,短期和长期抗生素治疗铜绿假单胞菌-呼吸机相关性肺炎的复合或单独结局(90天死亡率或呼吸机相关性肺炎复发)没有差异。
原始出处:
Adrien Bouglé.et al.Comparison of 8 versus 15 days of antibiotic therapy for Pseudomonas aeruginosa ventilator-associated pneumonia in adults: a randomized, controlled, open-label trial.Intensive Care Medicine.2022.https://www.esicm.org/icm-search/?id=doi:10.1007/s00134-022-06690-5#article
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#TENS#
51
#相关性#
23
#呼吸机#
39
#抗生素治疗#
42
#Med#
0
#治疗比较#
27