J Clin Oncol:alloHCT前调节化疗的强度对AML患者预后的影响
2020-01-04 QQY MedSci原创
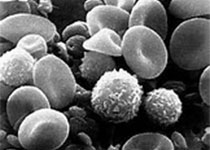
缓解期的急性髓系白血病(AML)患者仍有复发的风险,即使在异基因造血细胞移植(alloHCT)后。AML在alloHCT前可检测的残留病变(MRD)状态已被证实具有预后意义。对于MRD检测阳性的AML患者,改变alloHCT调节方案的强度是否可以预防复发,提高生存率,目前尚不清楚。本研究对一个III期临床试验的髓系恶性患者调节化疗前的血液中的13个AML常见突变基因进行深度靶向测序,在该试验中,所
本研究对一个III期临床试验的髓系恶性患者调节化疗前的血液中的13个AML常见突变基因进行深度靶向测序,在该试验中,所有获得形态学完全缓解的成人患者被随机分至清髓调节组(MAC)或减剂量调节组(RIC).
MAC组和RIC组分别有32%和37%的患者未检测到任何突变;这些组患者的存活率相近(3年总体存活率[OS] 56% vs 63%,p=0.96)。在携带一个可检测突变(NGS阳性)的患者中,MAC组和RIC组的复发率和存活率均具有显著差异(3年累积复发率 19% vs 67%,p<0.001;3年OS 61% vs 43%,p=0.02)。对NGS阳性患者进行多变量分析显示,根据疾病风险和供体校正后,与MAC相比,RIC与复发率升高(风险比HR 6.36)、无复发存活率降低(HR 2.94)和OS降低(HR 1.97)显著相关。AML MRD模型也显示,对检测呈阳性的患者,MAC优于RIC。
本研究表明对于alloHCT前MRD阳性的AML患者,MAC优于RIC,可提高患者的存活率。
原始出处:
Christopher S. Hourigan, et al.Impact of Conditioning Intensity of Allogeneic Transplantation for Acute Myeloid Leukemia With Genomic Evidence of Residual Disease.Journal of Clinical Oncology. December 27, 2019
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#alloHCT#
24
#患者预后#
33
#Oncol#
28
#ALL#
0
#HCT#
32
谢谢梅斯分享这么多精彩信息
53