Radiology:双能量CT碘浓度评价胰十二指肠切除术后胰瘘
2022-08-15 shaosai MedSci原创
双能量CT(DECT)是CT领域的一个进步,有利于绝对碘定量和基于多物质分解算法的脂肪分数分析。
众所周知,术后胰腺瘘(POPF)是胰腺十二指肠切除术后最常见且可能危及生命的并发症。对POPF进行准确的风险预测和分层可提示外科医生有选择地使用预防措施以减少并发症的发生。瘘管风险评分在估计POPF发展方面起着核心作用,该评分将公认的变量,包括诊断或病理结果、胰腺导管大小、胰腺纹理和估计失血量,纳入一个临床相关的评分系统。然而,这个评分是一个术中风险指标,取决于外科医生的主观估计。因此,需要建立一个准确且易于使用的术前识别方法以进行POPF高风险患者的识别。
术前成像的几个形态特征已被多项研究证明与POPF有关,包括胰腺厚度、残余体积和主胰管直径。据报道,胰腺脂肪变性和无纤维化会软化腺体,因此与发展POPF的高风险有关。因此,临床花了很多精力试图用术前的MRI来预测POPF的风险,方法包括扩散加权成像评估体内不相干运动的灌注分数、T1加权MRI评估信号强度比、MR弹性成像和磁化转移成像评估胰腺硬度。然而,MR弹性成像昂贵且成像复杂,而磁化转移成像并不是一种广泛可用的术前评估。虽然us弹性成像十分方便,但缺乏可重复性是其主要缺点。
双能量CT(DECT)是CT领域的一个进步,有利于绝对碘定量和基于多物质分解算法的脂肪分数分析。目前,DECT研究的一个重要领域是评估碘和脂肪值。但据我们所知,使用DECT来估计POPF风险在文献中还没有得到很好的证实。
近日,发表Radiology杂志的一项研究评估了术前DECT对碘浓度(IC)和脂肪部分的量化以实现POPF的预测,并进一步评估了潜在的组织病理学变化。

本项回顾性研究纳入了2020年1月-2020年12月期间接受胰十二指肠切除术和DECT(包括胰腺实质、门静脉和延迟相扫描)的患者。使用逻辑回归分析法分析了DECT得出的定量IC和脂肪分数以及增强图像的CT衰减值与POPF风险的关系。将IC的预测性能与CT值的预测性能进行了比较。用多变量线性回归分析评估了IC的组织病理学基础。
共有107名患者(中位年龄,65岁;四分位数范围,57-70岁;56名男性)被纳入研究。其中,23人(21%)患有POPF。胰腺实质与门静脉期IC比值(调整后的几率比[OR],13;95%CI:2,162;P < .001)是POPF发生的独立预测因素。胰腺实质-门静脉期IC比值预测POPF的准确性高于相同阶段的CT值比值(78% vs 65%,P < .001)。胰腺实质-门静脉期IC比值与胰腺纤维化独立相关(β=-1.04;95%CI:-0.44,-1.64;P=.001)。
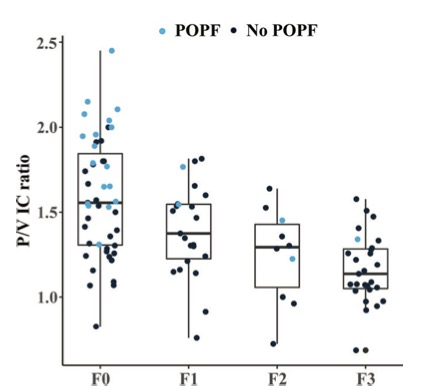
图 盒须图显示胰腺实质期与门静脉期的碘浓度比值(P/V IC比值)与纤维化显著相关(r = -0.529,P , .001)。框内表示上下四分位数,框内横线表示中位数,晶须表示范围
本研究表明,使用双能量CT(DECT)测定的术前定量碘浓度可作为胰十二指肠切除术患者术后胰瘘(POPF)的客观术前影像标志。本研究结果对外科医生在识别手术前POPF的高风险患者,从而改善个人围手术期护理和术中决策起到了重要的指导作用。
原文出处:
Hong-Yuan Shi,Zi-Peng Lu,Ming-Na Li,et al.Dual-Energy CT Iodine Concentration to Evaluate Postoperative Pancreatic Fistula after Pancreatoduodenectomy.DOI:10.1148/radiol.212173
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#切除术#
61
#十二指肠#
45
#评价#
49
#胰瘘#
38
#浓度#
51