NEJM:因心衰住院的老年患者身体康复评估
2021-07-15 MedSci原创 MedSci原创
在因急性失代偿性心力衰竭住院的老年患者不同人群中,早期、过渡性、定制化、渐进式康复干预包括多个身体功能领域,比常规护理更能改善身体功能。
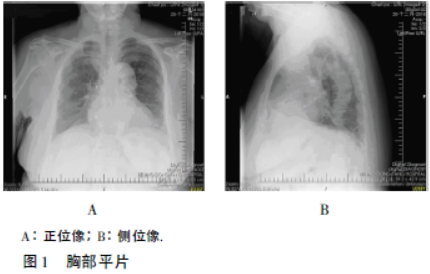
因急性失代偿性心力衰竭住院的老年患者身体虚弱、生活质量差、恢复延迟和频繁再住院的发生率很高。但解决该人群身体虚弱的干预措施尚未明确。 近日,顶级医学期刊NEJM上发表了一篇研究文章,研究人员进行了一项多中心、随机、对照试验,以评估过渡性、定制化、渐进式康复干预,其中包括四个身体功能领域(力量、平衡、移动性和耐力)。在因心力衰竭住院期间或之后早期开始干预,并在出院后继续进行36次门诊治疗。该研究的主要结局是3个月时短期身体机能评估得分(总分范围为0到12,得分越低表示身体机能障碍越严重)。该研究的次要结局是任何原因的6个月再住院率。 该研究共有349名患者接受了随机化分组;175人被分配到康复干预组,174人被分配到常规护理组(对照)。基线时,各组患者的身体功能明显受损,97%的患者伴有体弱或体弱前状态;每组合并疾病的平均数量为5个。干预组患者保留率为82%,干预组的依从性为67%。在调整基线短体能系列评分和其他基线特征后,干预组在3个月时短体能系列评估的最小二乘均值(±SE)得分为8.3±0.2,对照组为6.9±0.2。平均组间差异为1.5;95%置信区间[CI]为0.9至2.0;P&
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#心衰住院#
40
学习了
68
学习了
75
谢谢 学习了
62
谢谢 学习了
71
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
59
学习
36
我也同意
28
👍
31