BLOOD:好消息!ISAtuximab 联合地塞米松治疗复发/难治性多发性骨髓瘤可提高ORR
2021-03-05 MedSci原创 MedSci原创
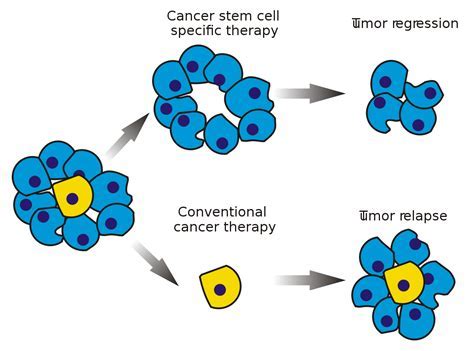
昨日,BLOOD发布Ⅱ期研究结果,显示在接受过中位数为4条治疗路线的骨髓瘤患者中,向ISAtuximab中添加地塞米松可使ORR从23.9%提高至43.6%。地塞米松改善了ISAtuximab的疗效,
昨日,BLOOD发布Ⅱ期研究结果,显示在接受过中位数为4条治疗路线的骨髓瘤患者中,向ISAtuximab中添加地塞米松可使ORR从23.9%提高至43.6%。地塞米松改善了ISAtuximab的疗效,对安全性没有不利影响,研究提供证据支持使用这种联合方案。

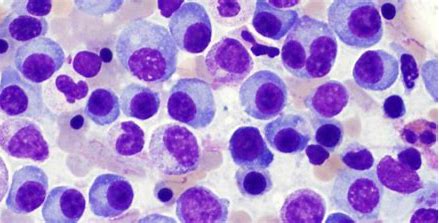
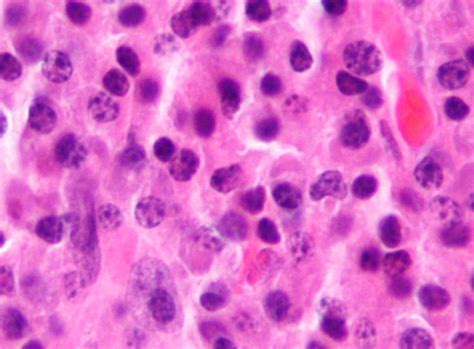
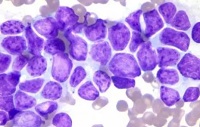
这项Ⅱ期研究评估了ISAtuximab单药治疗或联合地塞米松治疗复发/难治性多发性骨髓瘤(RRMM)的疗效和安全性。这些患者接受免疫调节药物(IMiD)和蛋白酶体抑制剂(PI)治疗无效,或接受过≥3种IMID和PI的先期治疗。
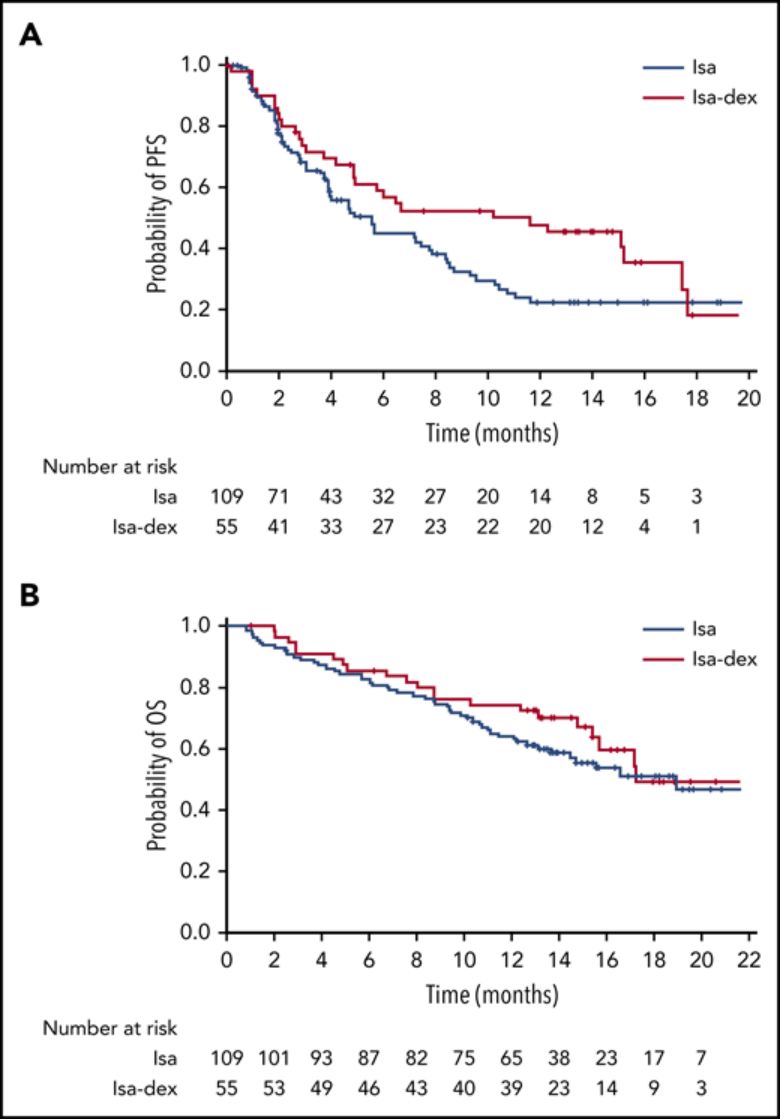
研究共纳入164名患者,其既往接受过中位数为4条治疗路线(2-10)。患者接受中位数分别为5(1-24)个和7(1-22)的治疗周期。截止数据时,109名患者中有13名(11.9%)和55名患者中有15名(27.3%)仍在ISA和ISA-Dex组接受治疗。
该研究无权在治疗组之间进行比较。但是,ISA组ORR为23.9%,ISA-Dex组ORR为43.6%在ISAtuximab单药治疗中加入地塞米松导致ORR显着增加(OR 0.405,95%CI 0.192-0.859;P=0.008)。
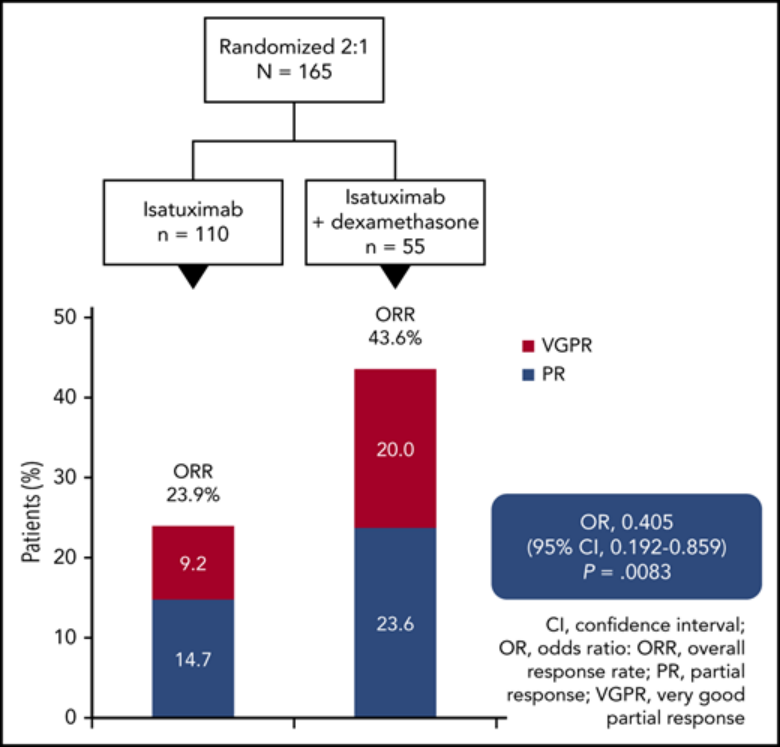
ISA组的PFS和OS分别为4.9个月和18.9个月,ISA-Dex组则分别为10.2个月和17.3个月。反应深度得到改善,并有PFS增加的证据(危险比[HR],0.677; 95%CI,0.440 -1.043;P<0.04)。部分患者获得PR(ISA,14.7%;ISA-Dex,23.6%),或是非常好的部分反应[VGPR;ISA,9.2%;ISA-Dex,20.0%]。这项研究中没有患者达到CR。但是,由于ISAtuximab对M蛋白测量的干扰,实际CR率可能会被低估。
ISA和ISA-dex的OS随访中位数持续时间分别为12.9(1-23)和13.4(1-24)个月。
根据ISA臂中50例死亡(占患者的45.9%)和ISA-dex臂中22例死亡(占患者的40.0%)来评估OS。两组OS中位数较接近,ISA和ISA-dex的OS中位数分别为18.9个月(95%CI,13.6-23.1)和19.3个月(95%CI,15.4-未达到)。)ISA和ISA-dex在12个月时的OS分别为63.5%(95%CI,54.4-72.7)和73.8%(95%CI,62.0-85.6)。
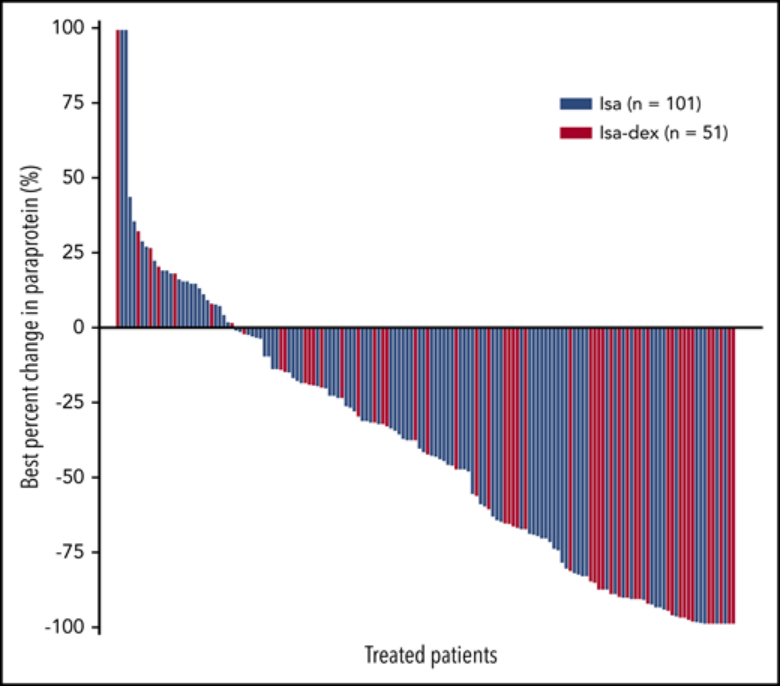
在基线后副蛋白评估≥1的患者中,37.1%(36/97)Isa组37.1%患者和58.0%(29/50)的Isa组患者降低≥50%。Isa组中的2名患者和Isa-dex组中的5名患者的M蛋白降低了100%。尽管Isa组中有2例患者和Isa-dex组中有5例患者的M蛋白降低了100%,但没有记录CR。但是,治疗性抗体干扰免疫评估和血清蛋白电泳分析用于反应评估可能会导致CR和VGPR的低估。
超过91%的患者出现≥1级的治疗紧急AE(TEAE)。最常见的不良事件输液反应(大多数为1、2级)和血液学异常。两组3级或更高级别感染的发生率相似,分别为22.0%和21.8%。
总而言之,在ISAtuximab中加入地塞米松可提高缓解率和改善生存结果,且不会对安全性产生不利影响。
在这项研究中,使用ISA-dex的ORR为44%,与pomalidomide +地塞米松(33%ORR),28 carfilzomib +地塞米松(55%),29 selinexor和dexamethasone(22%)观察到的临床反应率相比具有优势。

地塞米松改善了ISAtuximab治疗RRMM的疗效,对安全性没有不利影响。这项研究提供了将地塞米松与ISA有效联合治疗的理由。
原始文献:
Meletios Dimopoulos, Sara Bringhen , Pekka Anttila, et al. ISAtuximab as monotherapy and combined with dexamethasone in patients with relapsed/refractory multiple myeloma. Blood (2021) 137 (9): 1154–1165.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#mAb#
22
#多发性#
31
#isatuximab#
35
#难治性#
27
#ORR#
26