Clin Cancer Res:尼拉帕利在携带BRCA1/2胚系突变的晚期乳腺癌的疗效
2021-10-18 Nebula MedSci原创
尼拉帕利在既往治疗不超过2线化疗的HER2阴性的携带gBRCAm的晚期乳腺癌患者中具有治疗活性
携带BRCA1/2胚系突变 (gBRCAm) 的乳腺癌女性对铂类化疗和PARP抑制剂敏感,后者靶向DNA修复中的潜在缺陷。尼拉帕利(Niraparib)是一种有效的口服选择性PARP抑制剂,已被证明对卵巢癌和前列腺癌有效。
BRAVO试验是一项随机、开放标签的3期试验,旨在评估尼拉帕利用于携带BRCA1/2胚系突变(gBRCAm)的晚期乳腺癌患者的活性。
招募了既往治疗不超过2线化疗的HER2阴性的携带gBRCAm的晚期乳腺癌患者,随机(2:1)分至尼拉帕利组和医生决定的化疗组(PC;艾日布林、卡培他滨、长春瑞滨或吉西他滨单药治疗)。激素受体阳性肿瘤患者必须接受≥1线内分泌治疗并在转移性治疗期间出现进展或在(新)辅助治疗后 1 年内复发。主要终点是中心评估的无进展生存期(PFS)。次要终点包括总生存期(OS)、地方评估的PFS、客观缓解率(ORR)和安全性。
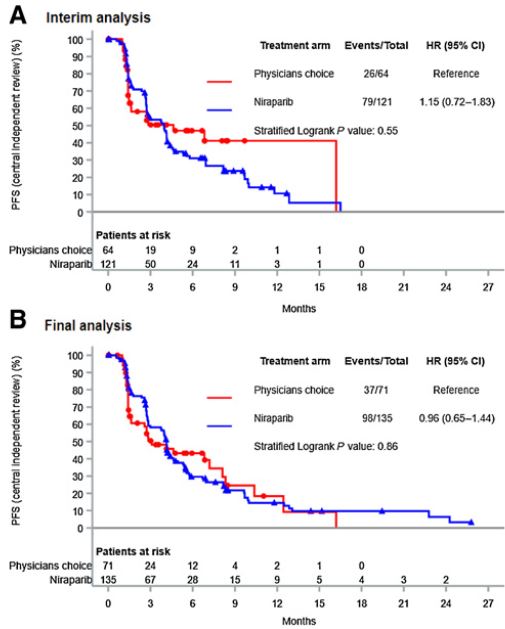
在中期和最终分析中,中心评估的PFS
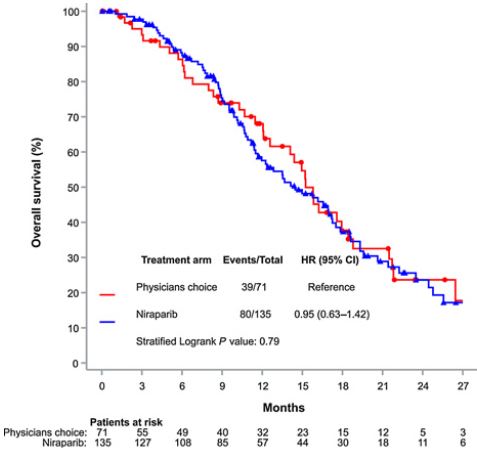
在预先计划的中期分析之后,招募因无效而停止(PC组地方和中心评估的PFS之间存在高度不一致,导致信息审查)。在最终分析中(中位随访时间为19.9个月),尼拉帕利组(n=141)中心评估的中位PFS为4.1个月,而PC组(n=74)的为3.1个月(风险比[HR] 0.96, 95% CI 0.65-1.44; p=0.86)。尼拉帕利组和PC组地方评估的中位PFS分别是5.0个月和3.1个月(HR 0.65, 95% CI 0.46-0.93)。尼拉帕利组和PC组的中位OS分别是14.5个月和15.2个月(HR 0.95, 95% CI 0.63-1.42; p=0.79)。尼拉帕利组和PC组的客观缓解率分别是35%和31%。
两治疗组的OS
综上所述,虽然有明确的证据表明尼拉帕利在该研究评估患者群体中具有治疗活性,但对照组中的信息审查阻止了对试验假设进行准确评估,。
原始出处:
Nicholas C. Turner, et al. Niraparib for Advanced Breast Cancer with Germline BRCA1 and BRCA2 Mutations: the EORTC 1307-BCG/BIG5–13/TESARO PR-30–50–10-C BRAVO Study. Clin Cancer Res October 15 2021 27 (20) 5482-5491; DOI:10.1158/1078-0432.CCR-21-0310
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#BRCA1#
49
#BRCA1/2#
0
#胚系突变#
38
#BRCA#
0
学习
62
#尼拉帕利#这是无效的结果
114
学习
88
学习一下
62
学习
67