Thorac Cancer:多中心回顾性研究评估dacomitinib(达可替尼)再挑战EGFR突变NSCLC患者的疗效
2022-05-24 yd2015 网络
在该真实世界研究中,达可替尼对之前EGFR- TKI治疗失败后EGFR突变的NSCLC患者是一种有价值的治疗选择。这种益处在具有21外显子突变的患者中尤其明显。
Dacomitinib(达可替尼)是一种第二代表皮生长因子受体(EGFR)酪氨酸激酶抑制剂(TKI)。在日本的真实世界中,EGFR-TKI治疗EGFR突变NSCLC患者进展后再挑战非常的常见。但是Dacomitinib(达可替尼)再挑战的疗效比较有限。近期,有相关结果发表在Thoracic Cancer杂志上。
该研究是在日本9个研究中心开展的多中心回顾性研究 (TOPGAN2020-02)。从TOPGAN组的9个参与机构筛选出43例患者。19外显子缺失(53.5%)和21外显子L858R(41.9%)是EGFR突变的主要亚型。只有2例(4.6%)患者存在罕见突变,包括G719X和L861Q。在达可替尼治疗前评估的31例患者(72.2%)不存在T790M突变。吉非替尼、阿法替尼和奥希替尼经常作为一线EGFR-TKI治疗。
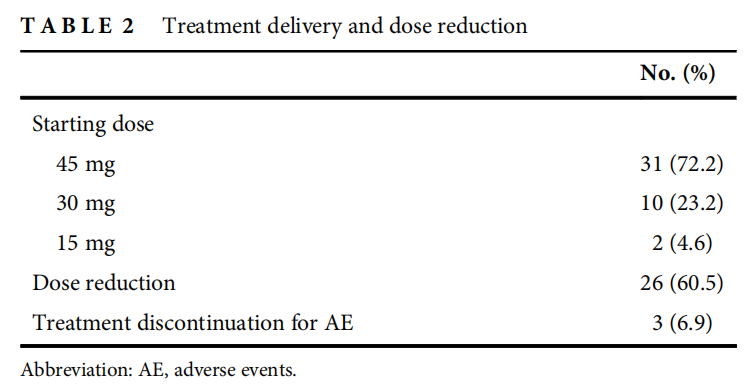
Dacomitinib的起始剂量分别为:31例(72.2%)45mg, 10例(23.2%)30mg, 2例(4.6%)15mg。根据到患者的年龄或PS,临床医生选择达可替尼的起始剂量。26例患者(60.5%)需要减少剂量。减少剂量的主要原因包括甲沟炎、腹泻、皮疹和口腔粘膜炎。
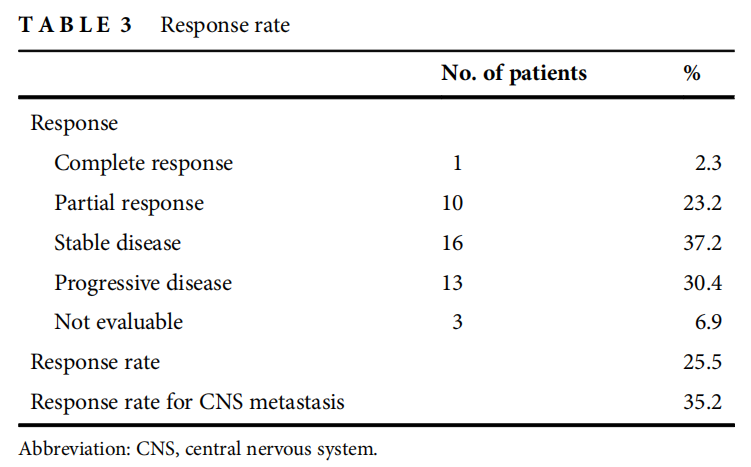
ORR为25.5%(95%置信区间[CI], 13.1 33.7),疾病控制率为62.7%。其中完全缓解(CR) 1例(2.3%),部分缓解(PR) 10例(23.2%),疾病稳定(SD) 16例(37.2%)。
中位无进展生存期(PFS)为4.3个月(95%置信区间[CI]为2.5 5.6)。总生存期(OS)为10.5个月(95% CI,未达到7.4个月)。
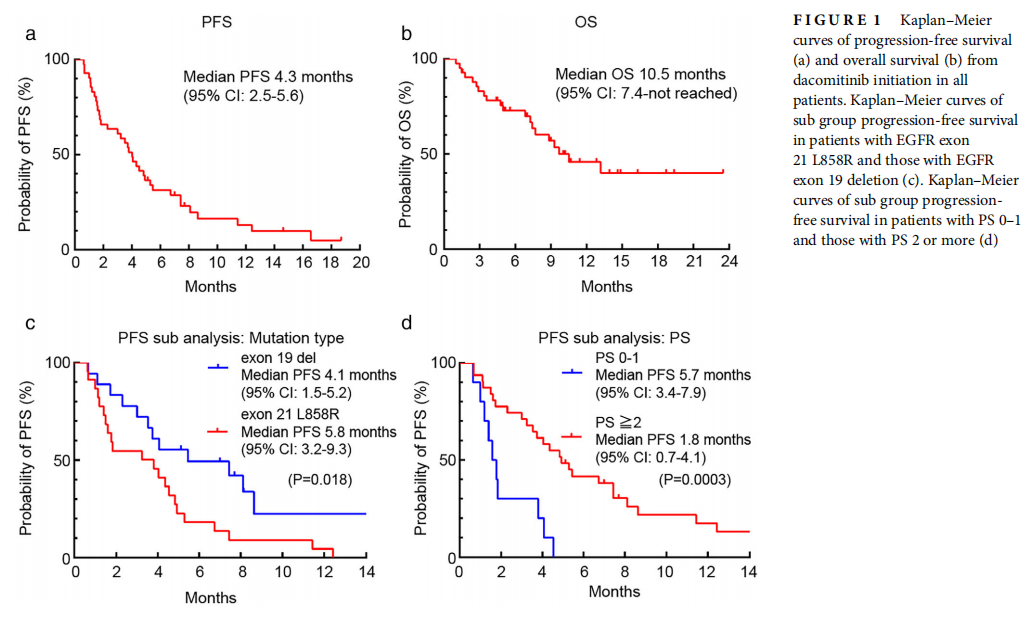
亚组分析显示,EGFR外显子21 L858R突变组患者的PFS长于EGFR外显子19缺失突变组(5.8个月vs 4.1个月)(p = 0.018)。相比之下,PS=2或更差患者的PFS短于PS=0-1患者(1.8个月vs 5.7个月,p = 0.0003)。低体重指数组(BMI <19)的PFS较BMI高组(BMI≥19)短(2.2 vs.5.0个月,p = 0.049)。其他因素无显著差异。尽管有26例患者因AEs而不得不减少达可替尼的剂量,但就PFS而言,它并不影响其疗效(减量组为5.1个月,无减量组为3.7个月)(p = 0.29)。

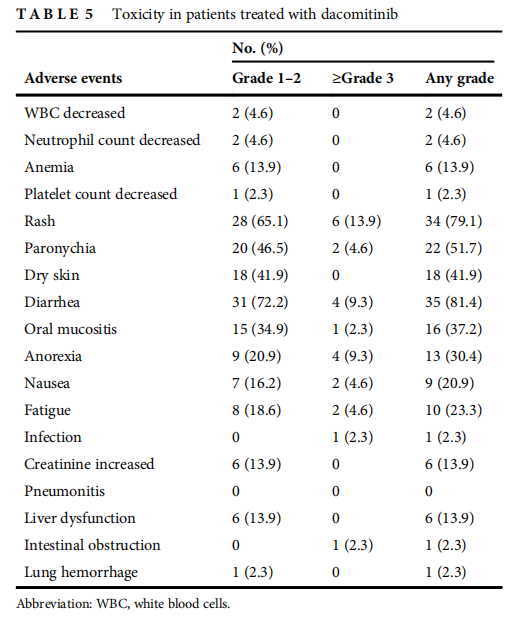
≥3级AEs包括皮疹(13.9%)、腹泻(9.3%)、厌食(9.3%)、甲沟炎(4.6%)。减少剂量的主要原因为甲沟炎、腹泻、皮疹和口腔黏膜炎。在达可替尼治疗期间没有患者发生肺炎。3例患者(6.9%)因毒性停止治疗。1例患者出现3级肠梗阻,该AE导致他们停止dacomitinib治疗。另外两名患者因食欲减退和腹泻停止治疗,其中一人因食欲减退和腹泻,另一人因甲沟炎和口腔粘膜炎延长而停止治疗。
综上,在该真实世界研究中,达可替尼对之前EGFR- TKI治疗失败后EGFR突变的NSCLC患者是一种有价值的治疗选择。这种益处在具有21外显子突变的患者中尤其明显。
原始出处:
Tanaka H, Sakamoto H, Akita T, Ohyanagi F, Kawashima Y, Tambo Y, Tanimoto A, Horiike A, Miyauchi E, Tsuchiya-Kawano Y, Yanagitani N, Nishio M. Clinical efficacy of dacomitinib in rechallenge setting for patients with epidermal growth factor receptor mutant non-small cell lung cancer: A multicenter retrospective analysis (TOPGAN2020-02). Thorac Cancer. 2022 May;13(10):1471-1478. doi: 10.1111/1759-7714.14415. Epub 2022 Apr 12. PMID: 35415873; PMCID: PMC9108073.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#SCLC患者#
46
#多中心#
34
#MIT#
42
#达可替尼#
35
#THORAC#
35
#Dacomitinib#
24
#NSCLC患者#
30
#GFR#
0
#回顾性研究#
32
#学习##心血管#
45