子宫内膜不典型增生和高分化子宫内膜癌保守治疗的随机对照试验 || 二甲双胍联合醋酸甲地孕酮(MA)与单一MA对照研究
2021-01-22 姚淑娟 张师前 张师前公众号
01概况与背景
01概况与背景
黄体酮治疗被广泛应用于子宫内膜不典型增生(AEH)和高分化子宫内膜样子宫内膜癌(EEC)年轻女性保留生育能力的保守治疗,仍有20-30%的患者未能达到CR需要切除子宫而丧失生育能力。增加剂量和延长治疗时间在提高疗效同时也带来更多副作用,降低依从性。因此,迫切需要一个在较短的治疗时间内能获得更好CR率的新方案。
基础和临床研究均支持在AEH和EEC患者保留生育治疗中使用二甲双胍,但尚无直接证据表明二甲双胍联合黄体酮治疗效果优于单一黄体酮。本文进行了一项前瞻性随机对照试验,以研究二甲双胍联合醋酸甲地孕酮(MA)与单用MA作为保留生育能力治疗AEH和EEC患者的疗效。
02研究方法
本研究为单中心、开放性、II期随机对照试验。150例(18-45岁)AEH或高分化EEC患者随机分为MA组(n=74)和MA +二甲双胍组(n=76)。首先将AEH或EEC患者分层,然后随机分为MA(160mg,口服,每日)或MA (160mg,口服,每日)+二甲双胍(500mg,口服,每日3次)两组。主要研究终点为16周内累积完全缓解(CR)率(16w-CR率);次要研究终点为30w-CR率和不良事件。
03研究结果
二甲双胍联合MA组16w-CR发生率高于MA组(34·3% vs 20.7%, OR=2.0, 95%CI=0.89 ~ 4.51, p=0.09), 102例AEH患者的16w-CR发生率差异有统计学意义(39.6% vs 20.4%, OR=2.56, 95%CI 1.06 ~ 6.21, p=0.04)。二甲双胍对非肥胖(51.4% vs 24.3%, OR=3.28, 95%CI=1.22-8.84,p=0.02)或胰岛素敏感(54.8% vs 28.6%,OR=3.04, 95%CI=1.03-8.97, p=0.04)的AEH女性亚组也有显著影响。次要终点结果未见显著性差异。
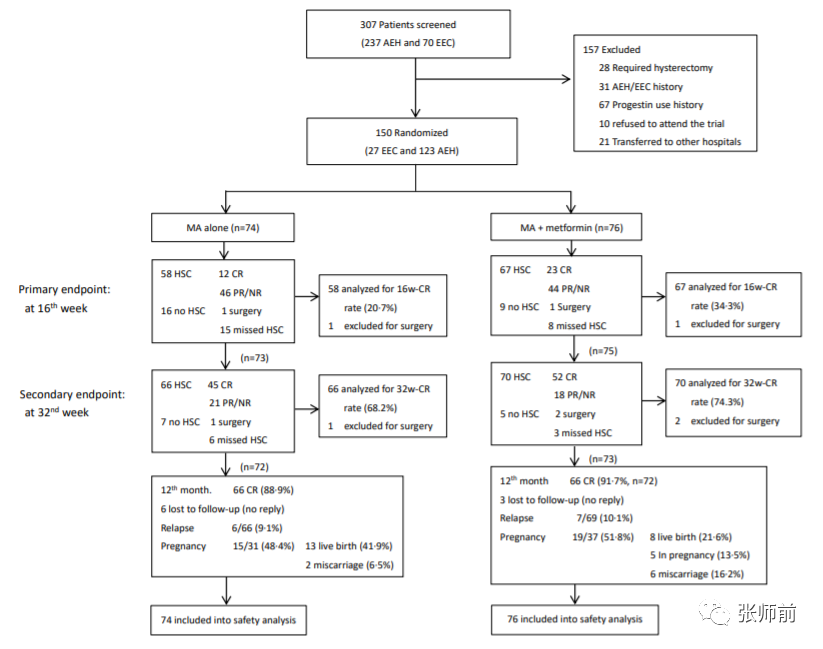
图1:试验流程
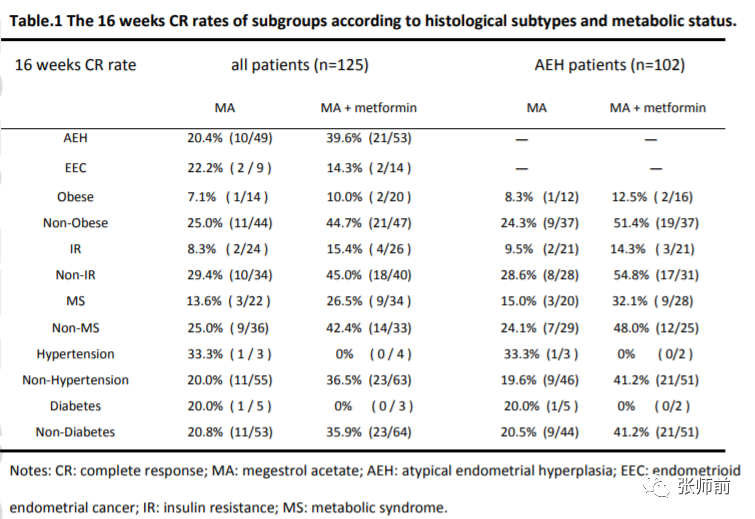
表1根据组织学亚型和代谢状态,测定各组16周的CR率
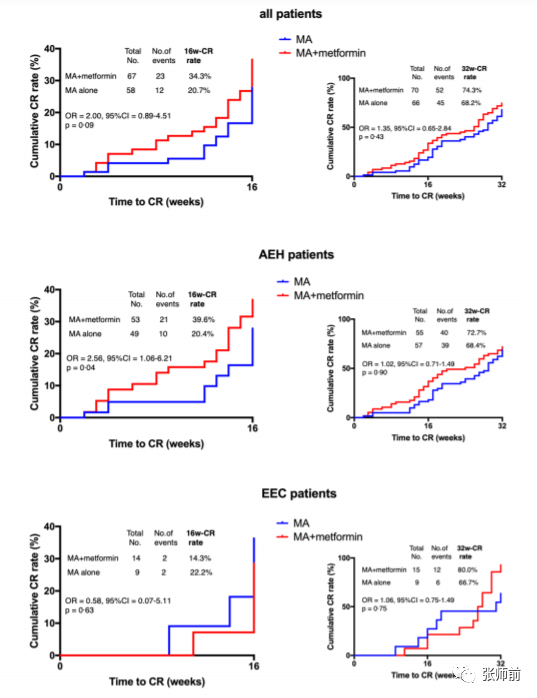
图2 所有患者及AEH和EEC患者亚组的16w-CR率和32w-CR率差异
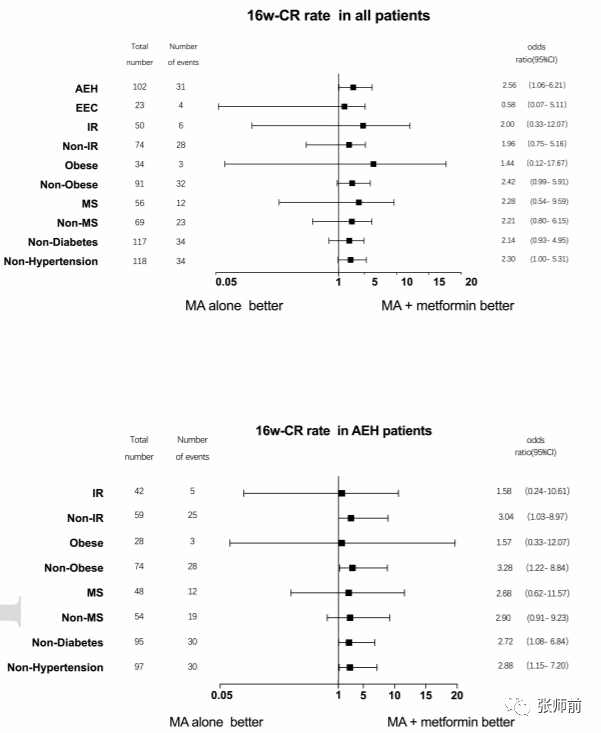
图3 根据组织学亚型和代谢状态进行亚组分析
04结论
在AEH患者中,二甲双胍联合MA作为一种保留生育能力的治疗,其早期CR率高于单独应用MA。
Bing-yi Yang, Yierfulati Gulinazi, Yan Du et al .Metformin plus Megestrol Acetate (MA)compared with MA alone as fertility-sparing treatment in patients with atypical endometrial hyperplasia and well differentiated endometrial cancer: a randomised controlled trial. BJOG
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#子宫内膜癌#
64
#不典型增生#
34
#对照试验#
33
#高分化#
30
#不典型#
37
#对照#
27
#内膜#
31
#随机对照试验#
36
#孕酮#
31
#保守治疗#
35