CGH: 维多珠单抗与肿瘤坏死因子拮抗剂在炎症性肠病患者中造成严重感染风险的差异比较
2022-01-28 MedSci原创 MedSci原创
炎性肠病又称炎症性肠病(IBD),为累及回肠、直肠、结肠的一种特发性肠道炎症性疾病。临床表现腹泻、腹痛,甚至可有血便。本病包括溃疡性结肠炎(UC)和克罗恩病(CD)。
维多珠单抗是继肿瘤坏死因子拮抗剂(抗TNF-α制剂)之后第一个被批准用于治疗炎症性肠病(IBD)的生物制剂。它可以通过与淋巴细胞α4β7整合素的特异性结合,影响淋巴细胞向胃肠道粘膜的迁移,从而发挥免疫调节的作用。其理论上的肠道选择性可能会降低肠道的免疫防御而导致相关不良事件的风险的增加,特别是严重感染的出现。维多珠单抗的相关研究中最常见的感染是上呼吸道感染。另外的研究则指出抗TNF-α制剂的使用也会造成一定程度的严重感染风险。
因此,本项研究旨在评估IBD 亚型和既往抗 TNF-α暴露情况下 IBD 患者使用维多珠单抗与抗 TNF 相关的严重感染风险。

为了完成本项研究,研究人员基于美国全国商业保险数据库和法国全国健康保险数据库的数据,将被诊断为克罗恩病 (CD) 和溃疡性结肠炎 (UC)的18岁或以上的患者纳入分析,他们开始使用维多珠单抗或抗 TNF药物被严格记录在案并进行统计学分析。然后在倾向评分匹配队列中估计了比较维多珠单抗和抗 TNF 的严重感染的风险比。
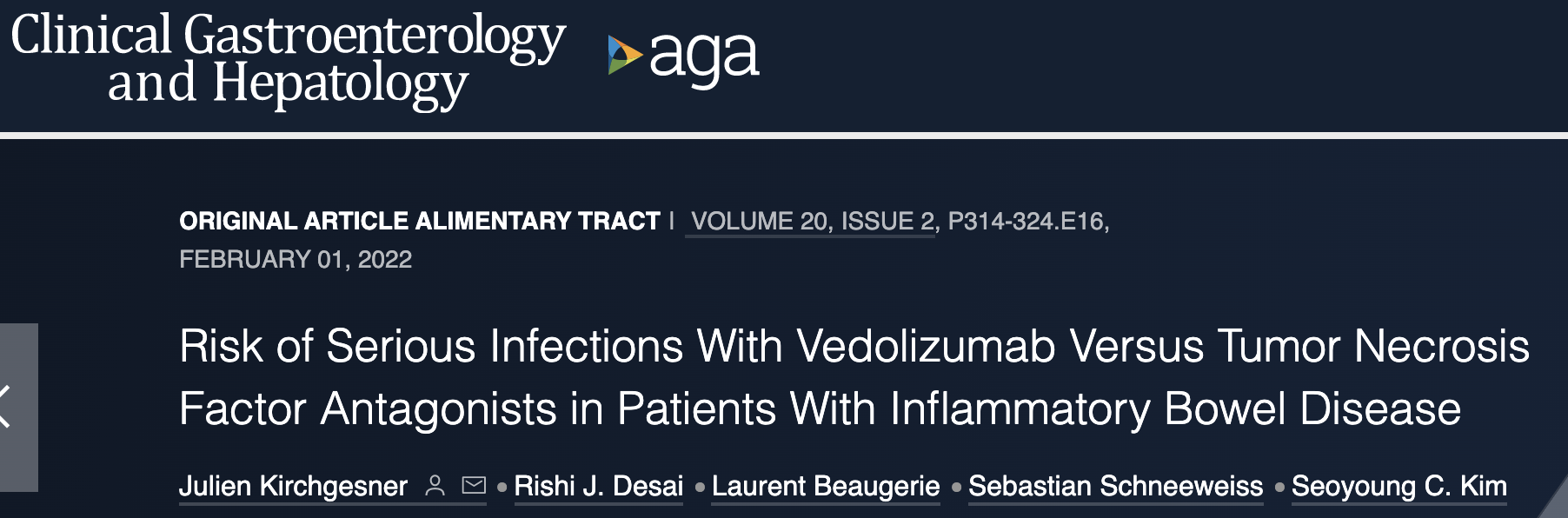
研究结果显示在倾向评分匹配后纳入了 8768 名维多珠单抗和 26,656 名抗 TNF治疗的患者,在37725人年的随访期间发生了893例严重感染事件。在整个 IBD 队列中,维多珠单抗(vedolizumab)和抗 TNF的使用患者出现严重感染风险没有差异(HR,0.95;95% CI,0.79-1.13),而 UC 患者中使用维多珠单抗(vedolizumab)的感染的风险明显降低(HR, 0.68;95% CI,0.50-0.93),但CD没有这样的现象(HR,1.10;95% CI,0.87-1.38)。在 UC 患者中,在排除胃肠道感染后,维多珠单抗始终与较低的严重感染风险相关(HR,0.59;95% CI,0.39-0.90)。
图:不同生物制剂造成感染的差异示意图
本项研究证实虽然与维多珠单抗相关的严重感染风险与抗 TNF 在整个 IBD 患者组中没有差异,但风险因 IBD 亚型而异,在 UC 患者中感染降低,但在 CD 患者不存在这样的现象。这些发现可能有助于阐明维多珠单抗在 IBD 治疗管理中的定位。
原始出处:
Julien Kirchgesner. Et al. Risk of Serious Infections With Vedolizumab Versus Tumor Necrosis Factor Antagonists in Patients With Inflammatory Bowel Disease. Clinical Gastroenterology and Hepatology.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CGH#
35
其理论上的肠道选择性可能会降低肠
61
学习了。
52
维多珠单抗
62
学习#学习#
62
#坏死#
35
#肿瘤坏死因子#
33
#拮抗剂#
46
#炎症性#
18
#严重感染#
28