Nat Med:中国慢病研究全新分析,降低坏胆固醇可预防脑梗
2019-03-30 卢芳 中国循环杂志
近日,中国慢性病前瞻性研究组在Nature医学子刊发表研究称,降低“坏胆固醇”低密度脂蛋白胆固醇(LDL-C)预防脑梗死净获益高,与年龄、高血压病史或心血管病史无关。
脑卒中是国人致死和致残的首位原因。
近日,中国慢性病前瞻性研究组在Nature医学子刊发表研究称,降低“坏胆固醇”低密度脂蛋白胆固醇(LDL-C)预防脑梗死净获益高,与年龄、高血压病史或心血管病史无关。
这项研究中,研究者首先利用近2万人的数据进行了巢式病例对照研究,结果显示,坏胆固醇越低,脑梗死风险越低,但脑出血风险增加。

图1 中国人群中不同LDL-C水平脑梗死和脑出血的发生风险
此外,研究者还发现,甘油三酯与脑卒中也有关系,但关联较弱;“好胆固醇”高密度脂蛋白胆固醇(HDL-C)则与脑梗死呈反比,而脑出血关联不大。
之后进行遗传学分析也表明,降低坏胆固醇可预防脑梗死。
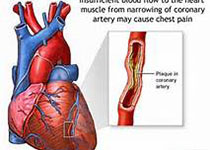
研究者还评估了使用他汀降低坏胆固醇的净获益,结果显示,降低坏胆固醇预防脑梗死及主要冠脉事件的风险,远可抵消脑出血的增加。
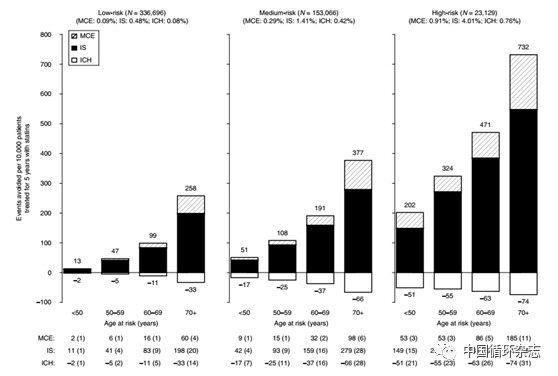
图2 不同血管风险者应用他汀类药物降低1 mmol/L LDL-C,以此估算的5年间每1万国人中可避免的脑梗死、主要心脏不良事件以及脑出血事件
这里值得注意的是,研究中将坏胆固醇LDL-C水平降低至1.7 mmol/L。
中国脑卒中报告指出,2016 年我国脑梗死发病率为276.75/10 万、脑出血发病率为 126.34/10 万。
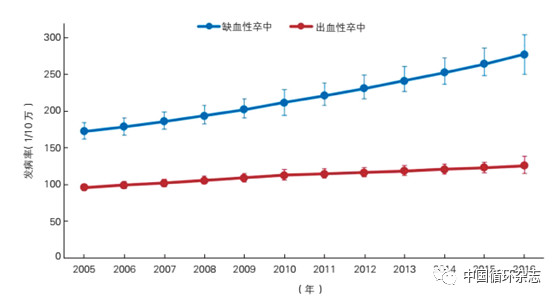
图3 2005~2016年中国不同类型脑卒中发病率
基于此,广泛应用降低坏胆固醇LDL-C的药物,比如他汀类以及PCSK9抑制剂具有重要意义,尤其是考虑到冠心病等心血管病时。
研究者强调,有些学者过多的担心降低LDL-C增加脑出血的风险,而实际上,他汀类药物的使用远远不够。
比如在中国慢性病研究及其他中国研究中,心血管病高危患者仅不到5%在规律使用他汀类药物,而在绝大多数西方国家使用率却在66%。
中国慢性病前瞻性研究共纳入全国10个地区512891位无心血管病史、无癌症病史的受试者,中位随访9年,共发生32869例脑梗死和8270例脑出血。
研究者对其中5475例脑梗死、4776例脑出血和6290例健康对照者进行了巢式病例对照研究。总体平均总胆固醇水平为4.6 mmol/L,LDL-C水平为2.4 mmol/L,HDL-C为1.2 mmol/L,甘油三酯为1.6 mmol/L。
原始出处:Luanluan Sun, Robert Clarke, Derrick Bennett, et al. Causal associations of blood lipids with risk of ischemic stroke and intracerebral hemorrhage in Chinese adults. Nat Med. 11 March 2019
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#慢病研究#
41
#Nat#
22
谢谢分享学习
55
#脑梗#
26
#Med#
30