IBD:克罗恩病患者使用5-氨基水杨酸药物的历史趋势分析
2021-03-28 MedSci原创 MedSci原创
克罗恩病(CD)是炎症性肠病的一种亚型,患者需要终生药物治疗,而手术通常只针对难治性或复杂疾病才有作用。
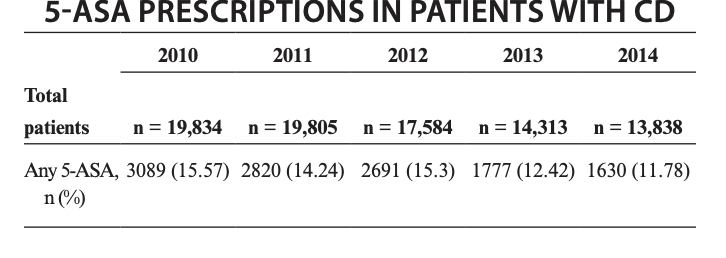
克罗恩病(CD)是炎症性肠病的一种亚型,患者需要终生药物治疗,而手术通常只针对难治性或复杂疾病才有作用。5-氨基水杨酸酯(5-ASA)药物用于治疗炎症性肠病已有悠久的历史,并且今天仍在广泛使用,5-ASA在溃疡性结肠炎中的有效性是显而易见的,然而,研究表明,对于克罗恩病(CD)的诱导或维持治疗几乎没有益处。本项研究旨在量化CD患者使用5-ASA处方的趋势。

研究人员通过美国商业保险数据库中的数据查询了2009年至2014年间年龄在18至65岁之间的CD患者的临床数据,然后按照年份计算了5-ASA药物处方使用率,5-ASA包括柳氮磺胺吡啶,美沙拉敏,olsalazine和balsalazide。回归模型用于检查处方率的逐年趋势,并确定与5-ASA使用相关的患者因素。

这项研究共收集了132804例CD患者,其中37.3%(n = 49,529)在研究期间接受了5-ASA处方治疗。从2009年到2014年,5-ASA的总体处方率从42.9%下降到30.0%(P <0.001)。与5-ASA的使用独立相关的患者因素包括年龄,男性,疾病并发症病等。最后作者说道尽管5-ASA在治疗克罗恩病中的有效性令人生疑,但约有三分之一的CD患者接受了5-ASA治疗;但是,从2009年到2014年,处方率呈现下降趋势也间接证明了其作用的不可靠。
原始出处:
Mohamed Noureldin. Et al. Trends of 5-Aminosalicylate Medication Use in Patients With Crohn Disease. Inflammatory Bowel Diseases.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#趋势分析#
39
#水杨酸#
45
#IBD#
32
#历史#
34
学到了很多东西谢谢老师
66
克罗恩
76