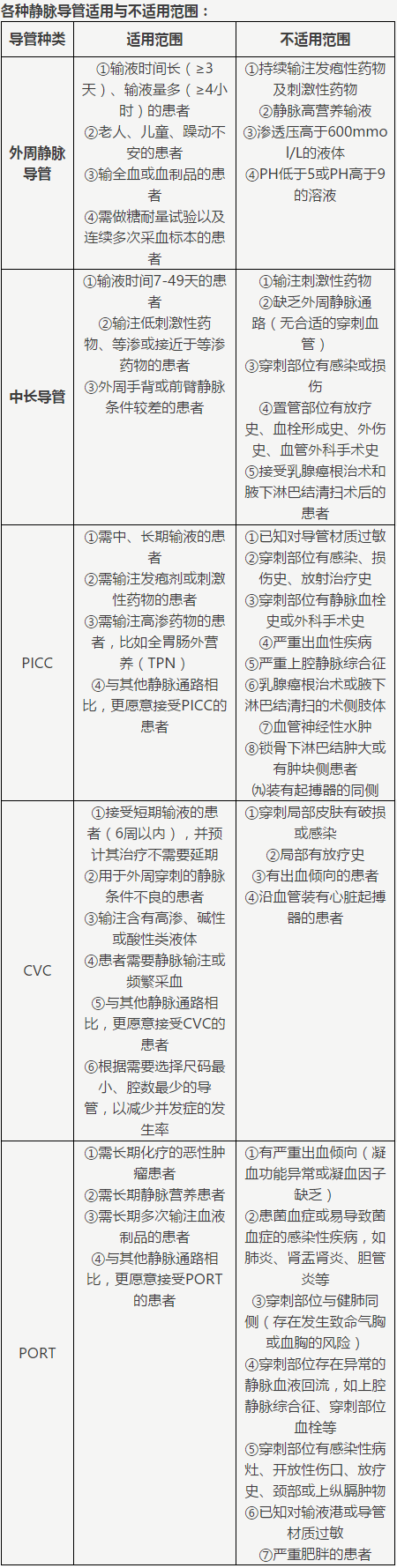
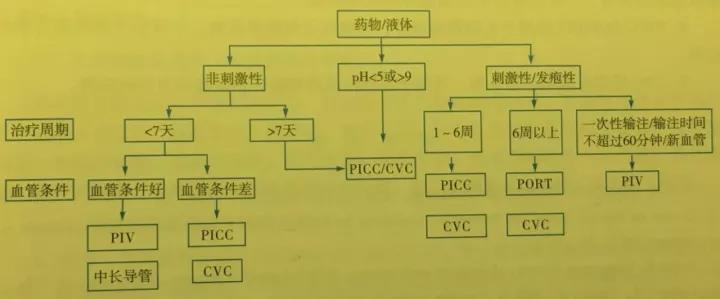
如何正确选择血管通路装置?
2017-11-24 徐梅 中国护理管理
在临床输液治疗中,如何根据患者的自身情况,治疗计划,药物性质,用药方法正确选择输液通路和输液器材,这是责任护士必需要认真思考的问题。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












谢谢分享学习了
55
#血管通路#
49
谢谢分享
95
好的方法.对患者负责!
103
谢谢分享学习了
99
谢谢分享.阅读
87
好好学习
105
学习
36
学习.谢谢分享
33
一起来讨论吧
37