JAHA:年龄对收缩压与心血管病风险相关性的影响研究
2020-07-18 MedSci原创 MedSci原创
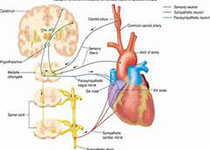
糖尿病患者收缩压(SBP)与心血管疾病(CVD)的关系尚不清楚。本研究旨在探讨SBP与CVD之间的年龄相关性。
糖尿病患者收缩压(SBP)与心血管疾病(CVD)的关系尚不清楚。本研究旨在探讨SBP与CVD之间的年龄相关性。
本研究纳入分析了180492名中国2型糖尿病成年患者,经过平均9.3年时间的随访,32545名患者发展为CVD,发病率为23.4/1000人年。在4个年龄组(<50、50-59、60-69和70-79岁)中,观察到SBP和CVD风险之间存在正相关和对数线性关系,但SBP对CVD的影响随年龄增长而减弱。年龄<50岁患者的CVD风险要比70-79岁患者高22%。每升高10毫米汞柱SBP,分别与12%(HR,1.12[95%CI,1.10-1.13])、11%(HR,1.11[95%CI,1.10-1.13])和20%(HR,1.20[95%CI,1.17-1.22])的所有复合心血管疾病事件、个体心血管疾病和心血管疾病死亡率的风险增加相关。
研究结果显示,对于糖尿病患者,收缩压与心血管病风险呈明显线性相关,年龄对这一关系有明显影响,与年龄较大的患者相比,年轻患者(<50岁)对这种相关性影响更大。
原始出处:
Eric Y et al.Age‐Specific Associations Between Systolic Blood Pressure and Cardiovascular Disease: A 10‐Year Diabetes Mellitus Cohort Study.JAHA.2020 July.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#相关性#
49
#血管病#
52
#收缩压#
45
#AHA#
43
很实用的研究
128
#心血管病#研究越来越细致
177