ATVB:补体激活酶MASP-2水平与静脉血栓栓塞的风险相关
2022-07-26 MedSci原创 MedSci原创
该研究结果表明,高血浆MSPS-2水平与未来发生静脉血栓栓塞的风险之间存在因果关系。
实验研究表明,补体激活酶-甘露糖结合凝集素相关丝氨酸蛋白酶2(MSPS-2)具有类似凝血酶的活性,能够抑制MSPS-2防止血栓形成。
近日,心血管领域权威杂志Arteriosclerosis, Thrombosis, and Vascular Biology上发表了一篇研究文章,在这项研究中,研究人员调查了血浆MSPS-2水平是否与未来静脉血栓栓塞(VTE)的风险相关,以及与MSPS-2水平相关的遗传变异是否与VTE风险相关。

研究人员进行了一项基于人群的嵌套病例对照研究,纳入了410例静脉血栓栓塞患者和842例来自挪威特罗姆瑟研究的年龄和性别匹配的对照者。研究人员使用Logistic回归估计了MSPS-2水平不同四分位数静脉血栓栓塞的比值比(OR),并采用全外显子组测序和蛋白质定量性状位点分析来评估与MSPS-2水平相关的遗传变异。研究人员进行了一项2个样本的孟德尔随机化研究,纳入了来自国际静脉血栓形成网络(国际静脉血栓网络发明联盟)的数据,以评估其因果关系。
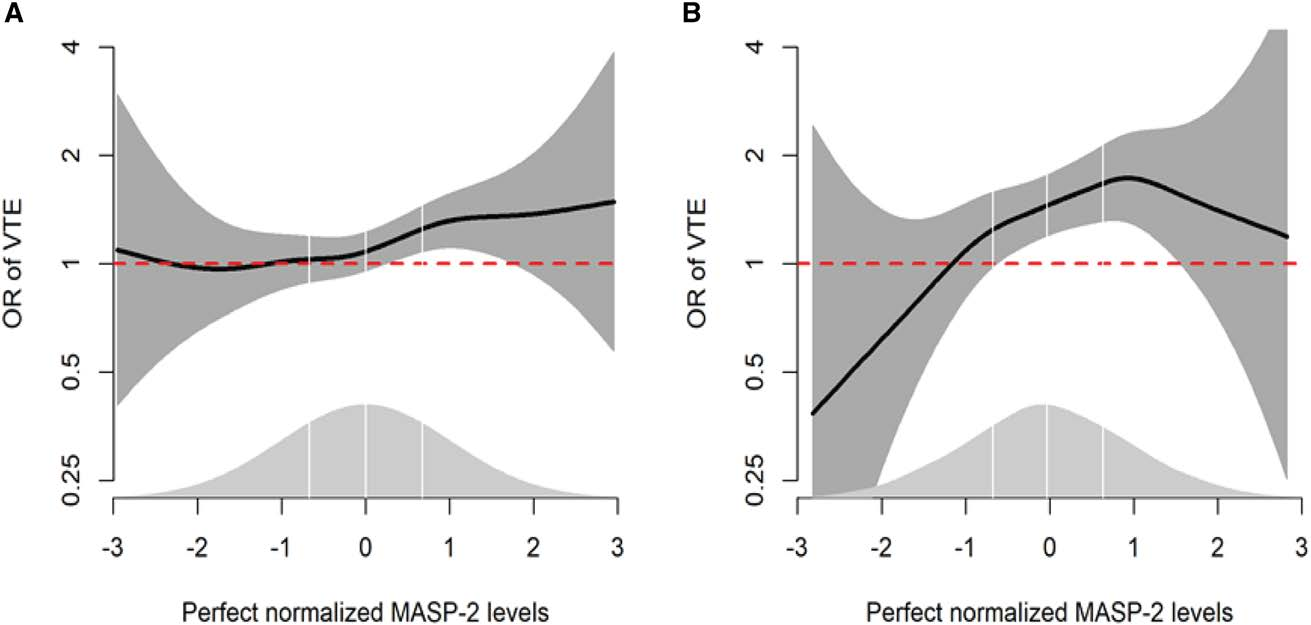
血浆MSPS-2水平在最高四分位的受试者与血浆MSPS-2水平在最低四分位的受试者相比,VTE的OR高出48%(OR为1.48[95%CI为1.06-2.06]),深静脉血栓的OR高出83%(OR为1.83[95%CI为1.23-2.73])。蛋白质数量性状位点分析显示,3个基因突变分别为rs12711521(小等位基因频率0.153)、rs72550870(小等位基因频率0.045;MASP2基因的错义变异)和rs2275527(次要等位基因频率0.220;外显子在邻MTOR基因变体)解释了39%MASP-2血浆浓度的变异。基因预测的MSPS-2每增加1个SDVTE的OR为1.03(95%CI为1.01-1.05,P=0.0011)。
由此可见,该研究结果表明,高血浆MSPS-2水平与未来发生静脉血栓栓塞的风险之间存在因果关系。
原始出处:
Christabel Esi Damoah.et al.High Levels of Complement Activating Enzyme MASP-2 Are Associated With the Risk of Future Incident Venous Thromboembolism.ATVB.2022.https://www.ahajournals.org/doi/10.1161/ATVBAHA.122.317746
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#静脉#
0
#静脉血#
42
#TVB#
37
#静脉血栓栓塞##补体#
77
#补体激活#
27