JCEM:接受甲状腺切除术的甲状腺癌患者心血管结局
2021-08-09 MedSci原创 MedSci原创
DTC患者发生房颤、CVD、心率加快和左心室质量增重的风险增加。
在一般人群中,甲状腺功能障碍与心血管疾病(CVD)风险增加有关;然而,分化型甲状腺癌(DTC)治疗,包括甲状腺切除术和注射促甲状腺激素抑制,是否会进一步增加CVD风险仍存在争议。

近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,该研究旨在评估DTC患者的CVD风险。
研究人员对MEDLINE、EMBASE和Web of Science进行了检索,并对评估DTC与心血管结局之间关联的观察性研究进行了回顾。研究人员排除了在DTC诊断前将CVD评估为合并症的研究,以及那些使用主动监测而不用甲状腺切除术作为干预的研究。当三项或更多研究报告了感兴趣的结局时,研究人员使用随机和固定效应模型对合并风险进行估计。研究人员评估了超声心动图和血液动力学参数。

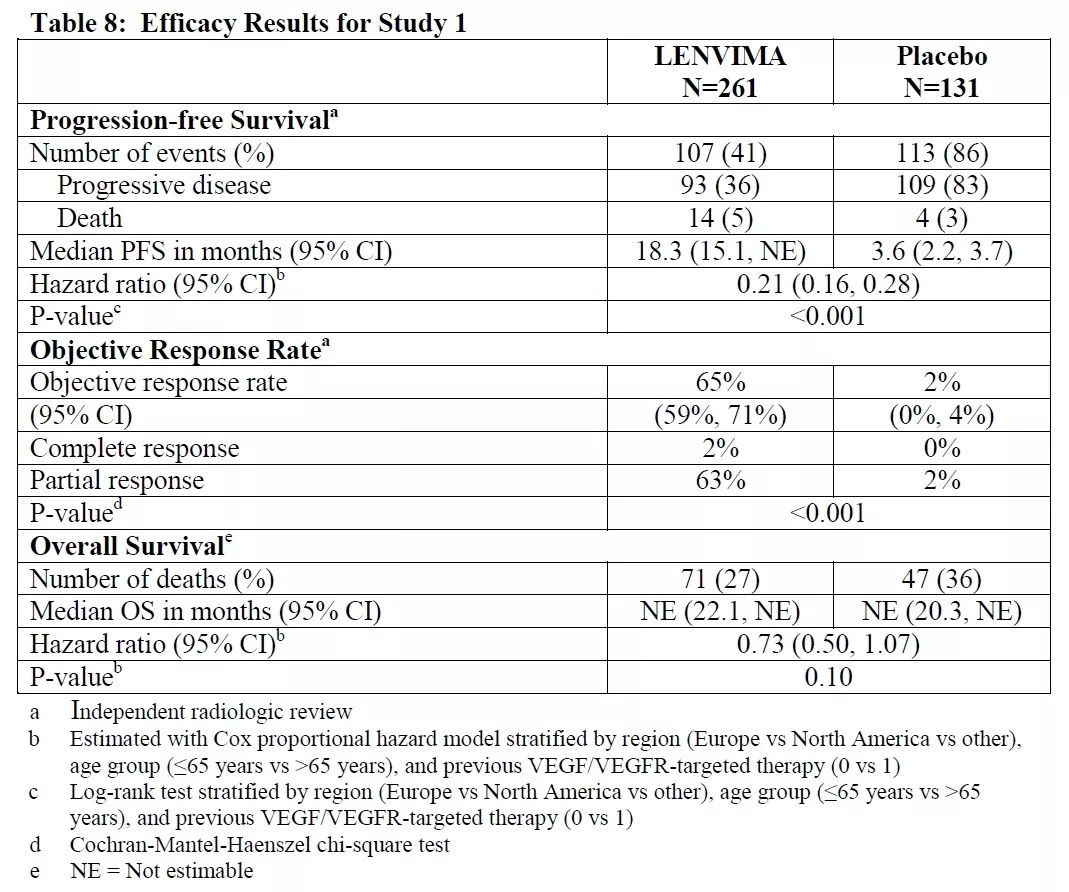
该定量分析中包括18项研究(193320例DTC患者和225575例健康对照者)。DTC与房颤(合并风险比[RR]=1.55[95%置信区间:1.30-1.84])、冠状动脉疾病(RR=1.10[1.00-1.21])、脑血管意外(RR=1.15[1.09-1.20])和全因死亡率(RR=1.95[1.03-3.69])风险增加相关。DTC与较高的舒张压(标准化平均差[SMD]为0.22[0.01-0.42])、心率(0.37[0.17-0.57])、左心室质量指数(0.66[0.45-0.88])和室间室间隔厚度(0.91[0.33-1.49])和早期至晚期心室充盈速度降低(-0.42[-0.79-(-0.05)])相关,但与射血分数无关。
由此可见,DTC患者发生房颤、CVD、心率加快和左心室质量增重的风险增加。
原始出处:
Eun Kyung Lee.et al.Cardiovascular outcomes in thyroid cancer patients treated with thyroidectomy: A meta-analysis.JCEM.2021.https://doi.org/10.1210/clinem/dgab576
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JCEM#
39
#JCE#
36
#切除术#
34
#心血管结局#
42
这是个令人担心的问题!
67
学习了
51
学习一下~
48
清楚!#心血管#
80