Spine:单独前路腰椎融合术效果可行
2014-07-29 李宁 丁香园
腰椎退变被认为是腰椎病或退行性椎间盘疾病。如果不处理,可能会导致腰椎狭窄、小关节退变和退行性腰椎滑脱,最终导致腰痛或坐骨神经痛。手术干预措施包括前路腰椎融合术、360°腰椎融合术、后路脊柱融合和椎间盘置换术。 一般来讲,如果存在椎间盘严重变性、脊柱不稳定、神经根压迫或非手术干预失败,融合手术就会被考虑。过去,后路腰椎融合辅以前路腰椎融合能够充分固定和融合,然而其手术发病率、术后疼痛、住院日均
腰椎退变被认为是腰椎病或退行性椎间盘疾病。如果不处理,可能会导致腰椎狭窄、小关节退变和退行性腰椎滑脱,最终导致腰痛或坐骨神经痛。手术干预措施包括前路腰椎融合术、360°腰椎融合术、后路脊柱融合和椎间盘置换术。
一般来讲,如果存在椎间盘严重变性、脊柱不稳定、神经根压迫或非手术干预失败,融合手术就会被考虑。过去,后路腰椎融合辅以前路腰椎融合能够充分固定和融合,然而其手术发病率、术后疼痛、住院日均增加。同时,360°腰椎融合具有花费和感染风险高的缺点。
令人惊讶的是,关于单独前路腰椎融合固定的评估,目前仍缺乏资料。于是,来自美国的Lammli学者等报道了应用单独前路腰椎融合术并人类骨形态蛋白2治疗一系列退变性腰椎疾病(L4-S1),该研究已在近期的Spine杂志上发表。
在该研究中,118例患者(58.5%为女性)获得了随访,平均年龄为43 ± 10岁。91.5%的患者为白种人。不吸烟患者占50%。
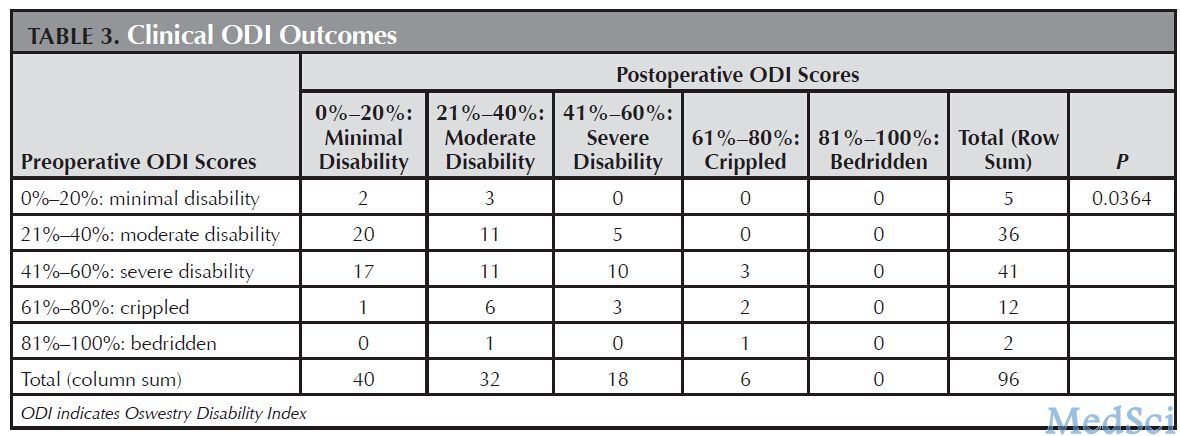
研究结果显示患者术后2年残疾障碍功能指数(ODI)和视觉疼痛得分(VAS)明显改善(P<0.01)。术后2年椎间盘高度较术前明显增高(P<0.01),而在毗邻节段椎间盘高度没有明显降低。107名患者(93.0%)获得满意的融合。在手术时间(单节段66分钟,双节段91分钟)、失血量(单节段48±30.9ml,双节段49.5±26.1 ml)和住院日(单节段2.6±0.8天,双节段3±0.6天)方面,单节段或双节段的前路腰椎融合术少于360°腰椎融合和椎间盘置换。
可见,前路腰椎融合固定术治疗退变性腰椎疾病是可行的,可认为是值得考虑的手术措施。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#腰椎融合术#
35
#Spine#
40
#腰椎融合#
0
#腰椎#
27
#融合#
21
#融合术#
32