Crit Care:较高和正常血压目标值对预防急性肾损伤的价值
2022-11-28 MedSci原创 MedSci原创 发表于上海
肾灌注不足是急性肾损伤(AKI)最常见的原因之一,特别是在休克和围手术期患者。预防AKI的最佳血压(BP)目标仍未确定。
肾灌注不足是急性肾损伤(AKI)最常见的原因之一,特别是在休克和围手术期患者。预防AKI的最佳血压(BP)目标仍未确定。
近日,危重病医学领域权威杂志Critical Care上发表了一篇研究文章,研究人员对现有的随机临床试验(RCT)结果进行了系统回顾和荟萃分析,以明确这一问题。
研究人员检索了Ovid Medline、EMBASE、Cochrane图书馆、SCOPUS、clinicaltrials.gov和WHO ICTRP,检索时间从数据库成立到2022年5月13日,以比较血流动力学不稳定患者(休克、心脏骤停后或手术患者)的高血压目标与正常血压的RCT。感兴趣的结果是干预后AKI发生率和肾替代治疗(RRT)率。两名研究人员独立筛选引用,并根据预定义的形式审查合格研究的全文。
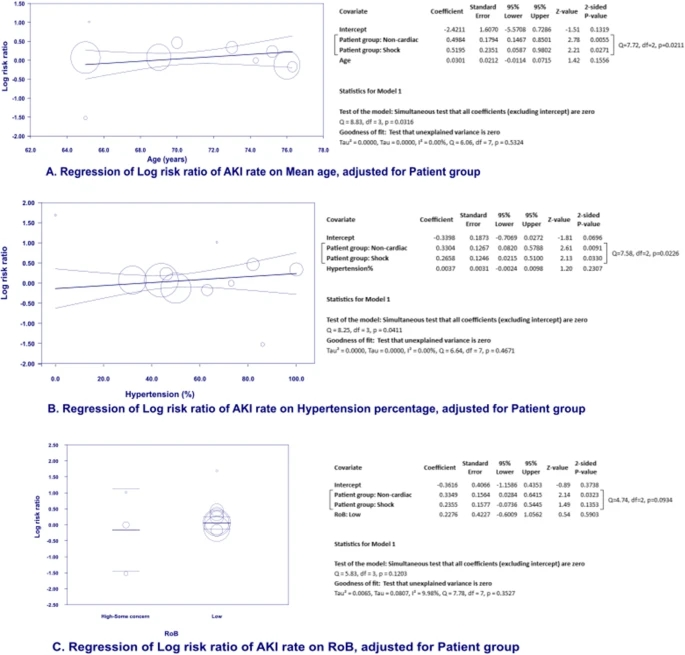
该研究共纳入了12项试验,共纳入了5759名参与者,休克、非心脏和心脏手术患者分别有3282(57.0%)、1687(29.3%)和790(13.7%)例患者。通过随机效应meta分析,与作为正常血压的较低平均动脉血压(MAP)目标值相比,在休克(RR[95%CI]=1.10[0.93, 1.29])、心脏手术(RR [95%CI]=0.87[0.73, 1.03])和非心脏手术患者(RR [95%CI]=1.25[0.98, 1.60])中,较高的平均动脉血压(MAP)目标值对AKI发生率没有显著影响。然而,在既往伴有高血压的休克患者中,以MAP高于70 mmHg为目标值可显著降低RRT风险,RR [95%CI]=1.20 [1.03, 1.41],p<0.05。
由此可见,在休克或围手术期患者中,较高的MAP目标值可能并不优于正常血压,但既往伴有高血压的休克患者除外。需要进一步的研究来评估较高MAP目标值对在常见的血流动力学不稳定的高血压患者中预防AKI的作用。
原始出处:
Phu Nguyen Trong Tran.et al.Higher blood pressure versus normotension targets to prevent acute kidney injury: a systematic review and meta-regression of randomized controlled trials.Critical Care.2022.https://cardiab.biomedcentral.com/articles/10.1186/s12933-022-01692-5
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










结合临床,积极管理血压
32
转发学习
33
感谢分享
33
学习受益
26