Sci Rep: 成纤维细胞到尿路上皮细胞直接转化在受损泌尿膀胱粘膜再生中可能是需要的
2019-10-18 AlexYang MedSci原创
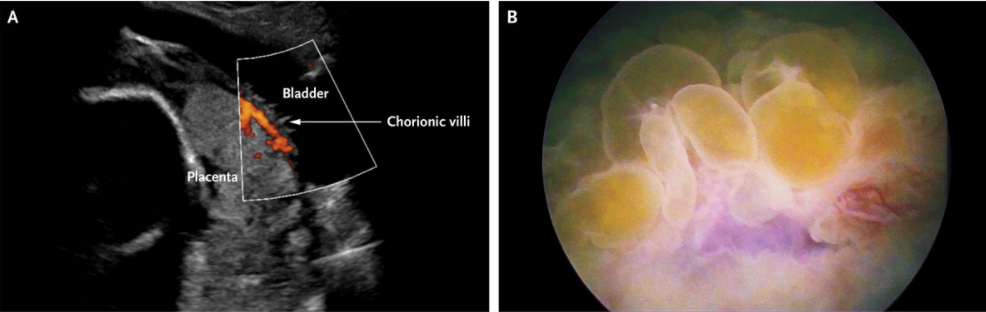
在尿路粘膜中,尿路上皮细胞在尿液渗出和细菌侵染中具有重要的作用,因此尿路上皮细胞的缺陷或者是损伤与泌尿系疾病相关,并且可能引起严重的问题。如果能够培养足够数量的功能尿路上皮细胞并移植到受损的尿路上皮中,该技术可能对患有泌尿道疾病的患者提供有利的影响。最近,有研究人员发现通过转化4个转录因子FOXA1,TP63, MYCL和KLF4 (FTLK),人类成年成纤维细胞能够转换成为尿路上皮细胞。上述直接
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#粘膜#
39
#成纤维细胞#
42
#纤维细胞#
0
#上皮细胞#
0