Arthritis Rheumatol:使用自身抗体和皮肤亚群建立系统性硬化症基于结局的疾病分类
2019-11-25 xiangting MedSci原创
这项研究强调了自身抗体、皮肤亚群和疾病病程在评估SSc发病率和死亡率中的重要性。
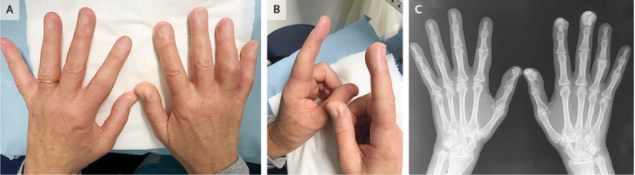
这项研究旨在描述系统性硬化症(SSc)患者自身抗体、临床表现与结局之间的关联。作者提出了一个包括抗体和皮肤亚群的新SSc分类。
使用生存分析评估抗体对器官疾病和死亡的影响。
该研究包括1325名受试者。ACA+局限性皮肤SSc组(lc)(n=374)的20年生存率最高(65.3%),而临床明显肺纤维化(csPF,8.5%)和硬皮病肾危象的发病率最低(SRC,0.3%),心脏SSc发病率低(4.9%),而肺动脉高压(PH)发病率与同期队列平均值相似。
抗Scl70+lcSSc组(n=138)和弥漫性皮肤SSc组(dc)(n=149)的csPF发病率最高(15年时分别为86.1%和84%)。20年时dcSSc组的生存率最低(32.4%),心脏SSc发病率第二高(12.9%),而lcSSc组的其他并发症很少见,PH发病率最低(6.9%),生存率第二高(61.8%)。
抗RNA聚合酶+组(n=147)的SRC发病率最高(28.1%)。抗U3RNP+组(n=56)的PH(33.8%)和心脏SSc发病率最高(13.2%)。
在有其他自身抗体的lcSSc患者中(n=295),SRC和心脏SSc的风险较低,而其他结局与队列平均水平相似。有其他抗体的DcSSc患者(n=166)预后较差,生存率倒数第二位(33.6%),并经常出现器官并发症。
这项研究强调了自身抗体、皮肤亚群和疾病病程在评估SSc发病率和死亡率中的重要性。该分类有助于疾病监测和临床试验设计。
原始出处:
Svetlana
I. Nihtyanova. Using autoantibodies and cutaneous subset to develop
outcome‐based disease classification in systemic sclerosis. Arthritis
Rheumatol. 04 November 2019.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#硬化症#
24
#Arthritis#
27
#系统性#
25
#ART#
39
#疾病分类#
32
#系统性硬化#
27