外伤性冠状动脉夹层竟在6年后才被发现 看医生怎样力挽狂澜
2017-11-10 胡大一 马长生 心脏病学实践2013
48岁男性患者,因“活动后胸闷气促3月余” 于2011年12月13日入院。经问诊得知患者6年前胸部被严重挤压但未进一步检查。改善心功能后行冠状动脉造影发现,患者有三支冠状动脉夹层,最终诊断为陈旧性下壁心肌梗死、缺血性心肌病。6年前的外伤是否是造成患者心功能恶化的主因? 3支冠状动脉同时夹层形成该如何治疗?详见以下病例——
48岁男性患者,因“活动后胸闷气促3月余” 于2011年12月13日入院。经问诊得知患者6年前胸部被严重挤压但未进一步检查。改善心功能后行冠状动脉造影发现,患者有三支冠状动脉夹层,最终诊断为陈旧性下壁心肌梗死、缺血性心肌病。6年前的外伤是否是造成患者心功能恶化的主因? 3支冠状动脉同时夹层形成该如何治疗?详见以下病例——
患者近3个月来逐渐出现活动后胸闷气促,步行50m或上一层楼梯即出现症状,休息后缓解,夜间需高枕卧位,伴有足踝部水肿。无发热,无咳嗽咳痰,无胸痛。当地医院“利尿”治疗后水肿消退,但仍感乏力,遂转来本院。
有高血压病史20年,最高血压180/100mmHg,不规则服药(珍菊降压片),近年来血压控制在120~130/70~80mm Hg左右。6年前在自家工厂操作时,不慎胸部被严重挤压,发生一过性晕厥,自行苏醒后感胸部疼痛,外敷“伤湿止痛膏”数天后缓解,未进一步检查。否认其他突发胸痛、胸部不适病史;无高脂血症、糖尿病、结缔组织病、关节肿痛病史;无吸烟、饮酒嗜好。
入院查体:P 90次/分,BP 120/70mmHg,精神尚可,体型正常,颈静脉充盈,胸廓无畸形、无压痛,双肺底少许湿性啰音,心界位于左侧第5肋间锁骨中线外0.5cm,心率90次/分,律齐,第一心音低钝,心尖区闻及2/6级收缩期杂音,双下肢无水肿。
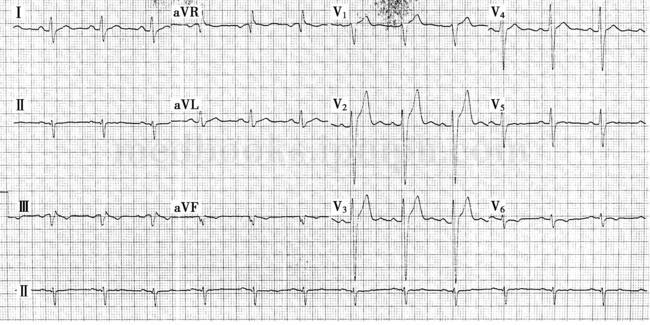
入院心电图示窦性心律,Ⅲ、avF导联病理性Q波伴T波倒置;胸前导联R波递增不良,V2~3导联ST段抬高,T波高尖,V5~6导联T波低平浅倒(图3)。Hotter示窦性心律,频发室性期前收缩16 751次,时呈二连律、三连律。心脏超声:左房室扩大伴左室多壁段收缩活动异常,下后壁局部室壁瘤形成(LVEDd 69mm,LVEDs 52mm,L VEF 39%)。总胆固醇:4.12mmol/L;甘油三酯:4.47mmol/L;HDL‐ch:0.98mmol/L;LDL‐ch:1.11mmol/L;CK‐MB:13U/L;CK‐M M:32.0U/L;hs CRP:1.6mg/L;cTnT:0.006ng/ml;N T‐proBNP:130.0pg/ml;FT3:5.6pmol/L;FT4:19.7pmol/L;s‐TSH:5.430μIU/ml。自身免疫抗体和血管炎性疾病相关指标均阴性。全身大中动脉CTA示胸腹主动脉轻度粥样硬化,未见其余血管夹层形成。
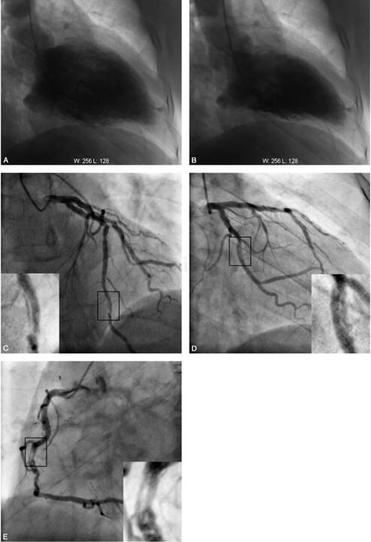
经改善心功能后,患者于2011‐12‐29行冠状动脉造影:前降支近中段长病变,发出第一对角支处狭窄70%。前降支远段线性夹层形成,狭窄70%;回旋支近段管壁不规则,远段夹层形成,狭窄80%;右冠状动脉血管扭曲,中段长程螺旋状夹层形成,狭窄80%。左室造影示:下壁及心尖部室壁瘤形成,LVEF20%(图4)。IV US检查证实前降支和回旋支夹层形成;超声导管无法通过右冠状动脉病变处。于前降支远段植入3.0mm×36mm Excel西罗莫司药物洗脱支架,回旋支远段植入3.0mm×24mm Excel西罗莫司药物洗脱支架,复查造影和IV US示支架扩张满意,贴壁良好,边缘无明显夹层,远端TIMI血流3级。建议择期行右冠状动脉介入治疗。
出院诊断:1﹒冠心病:陈旧性下壁心肌梗死,室壁瘤形成,三支冠状动脉夹层形成,PCI术后;2﹒缺血性心肌病、慢性心功能不全(NY H AⅢ级)。予阿司匹林、泰嘉、金络、雅施达、立普妥、安体舒通、欣康、万爽力、速尿、可达龙等治疗,出院半年后再次入院行右冠状动脉支架置入术,时诉症状有所改善,但复查心脏超声未见心脏功能明显改变。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#外伤性#
32
#冠状动脉夹层#
34
#动脉夹层#
37