肿瘤相关成纤维细胞(CAF)是肿瘤微环境(TME)的重要组成部分,具有多种功能,如细胞外基质(ECM)重塑、代谢和血管生成的调节,以及通过产生生长因子、细胞因子和趋化因子与癌细胞和浸润性免疫细胞的相互作用。
在TME环境中,CAF表现出具有相对特异性标记物的形态和功能转变,并具有促进肿瘤发生、发展和对多种治疗策略产生耐药性的作用,包括化疗、放疗、靶向治疗、抗血管生成治疗、免疫治疗和内分泌治疗。因此,CAF本身以及下游效应器和/或信号通路是优化抗癌治疗敏感性的潜在重要靶点。
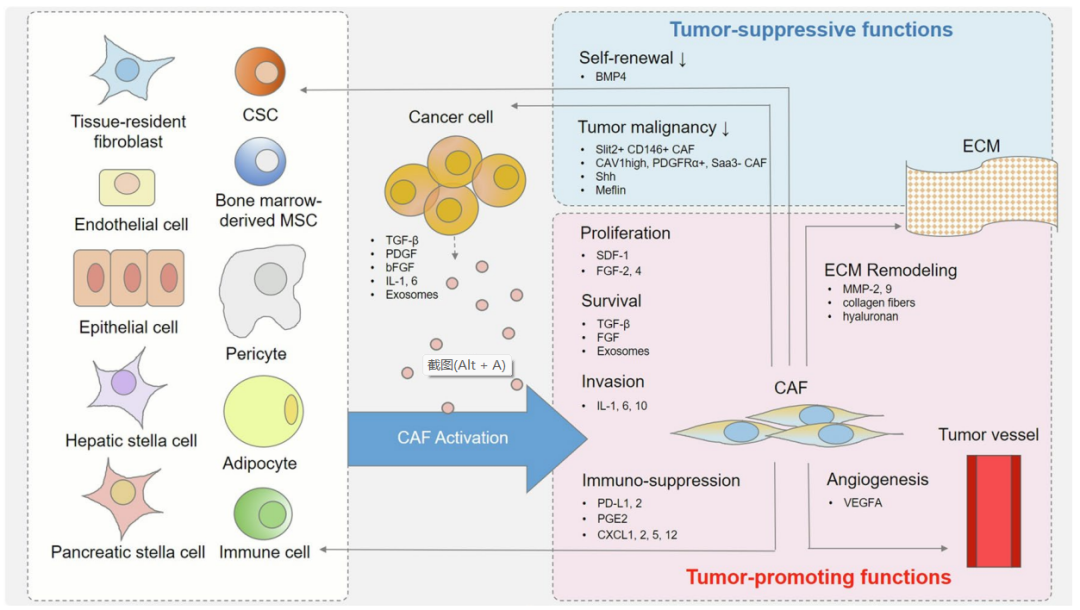
新的证据表明,CAF起源于异质细胞群体在各种内在和外在因素影响下的结构和功能改变。组织驻留的成纤维细胞、骨髓间充质干细胞(MSCs)、上皮细胞和内皮细胞可能通过TGF-β、上皮-间充质转化(EMT)或内皮-间充质转化(EndMT)转化为CAF。CAF也可以从脂肪细胞或周细胞的转分化进化而来,基质细胞缺乏维生素可能会诱导α-SMA的上调和向CAF的分化。此外,CAF可以从癌细胞在原发和转移部位招募的多种前体细胞中获得,包括癌症干细胞(CSCs)。
除了最初的异质性外,CAF激活的不同来源也会影响表型异质性。组织学上,活化的CAF呈纺锤状,有显著的核仁、粗面内质网、高尔基体、缝隙连接和细胞质肌丝。在这个阶段,激活的细胞通常以特定于环境的方式表现出广泛不同的生物标记物的表达。尽管并非仅限于CAF,但一些表面标记物的表达模式,如α-平滑肌肌动蛋白(α-SMA)、铁死亡抑制蛋白1(FSP1)、富含半胱氨酸的酸性分泌蛋白(SPARC)、血小板衍生生长因子β(PDGF-β)和整合素α11,可用于CAF的识别。
CAF的主要作用是以高度协调的模式重塑和再生组织。在TME的背景下,CAF通过创造一个促炎症、免疫抑制和富氧的微环境来促进肿瘤的发生和发展。在肿瘤发生的早期阶段,肿瘤源性IL-1β诱导CAF活化,以NF-κB依赖的方式协调促瘤炎症。此外,CAFs的免疫抑制特性通过促进免疫逃避促进肿瘤生长。一些CAF亚群可通过表达PD-L1或分泌前列腺素E2直接使免疫系统失活。除了对免疫细胞产生直接影响外,CAF还参与构建细胞外基质蛋白网络,作为治疗药物和免疫细胞到达肿瘤的物理屏障。此外,CAF通常会上调缺氧诱导的血管生成调节因子(HIAR)的表达,这可以增加CAF的运动性和血管内皮生长因子A(VEGFA)的分泌,并进一步促进血管生成,从而促进肿瘤的氧合和营养流动。
除了促进肿瘤的作用外,CAF在某些情况下还参与肿瘤抑制。例如,研究发现,在胰腺导管腺癌(PDAC)的基因工程小鼠模型中,清除CAF会导致低分化肿瘤和生存期缩短,这表明音猬因子驱动的CAF可以抑制肿瘤生长进展。进一步的研究表明,随着CSCs数量的增加,CAFs的缺失会导致侵袭性肿瘤,并降低体内生存率。最近,CD146+CAF、CAV1highCAF和PDGFRα+Saa3-CAF已被确定为乳腺癌中的肿瘤抑制性CAF亚群。
CAF与抗癌治疗的敏感性高度相关,根据Meads等人提出的分类法,CAF介导的耐药性可大致分为可溶性和分泌因子介导的耐药性(SFM-DR)以及细胞粘附介导的耐药性(CAM-DR)。SFM-DR由CAF产生的细胞因子、趋化因子、生长因子、外泌体和促结缔组织增生反应介导,这些反应可保护癌细胞免受药物诱导的凋亡,而CAM-DR则由癌细胞整合素粘附到基质成纤维细胞或ECM组分(如纤维连接蛋白、胶原和层粘连蛋白)介导。

一方面,在旁分泌调节因子的帮助下,包括细胞因子(TGF-β、TNF-α、IL-1等)、趋化因子以及由CAF和癌细胞分泌的生长因子,CAF有助于构建一个适合肿瘤血管生成、转移和治疗抗性的环境,从而有利于肿瘤生长。另一方面,作为TME的主要成分,CAF作为治疗屏障,在实体癌治疗中防止抗癌药物和免疫细胞浸润。
CAF在癌症发展过程中发挥的促瘤作用使其成为抗癌治疗的理想靶点。CAF导向的抗癌策略通常可分为靶向CAF的肿瘤促进功能、下游效应器和CAF激活表型的正常化。

抗CAF治疗主要集中在通过靶向特定表面标记物去除CAF,例如成纤维细胞活化蛋白(FAP)。以FAP+CAF为目标的DNA疫苗增加了CD8+和CD4+T细胞在肿瘤内的浸润。进一步的策略,如FAP-CAR-T细胞治疗和FAP靶向溶瘤腺病毒促进针对FAP+CAF的特异性免疫攻击,上调促炎细胞因子,增加抗原呈递、T细胞功能以及转运,从而增强抗肿瘤疗效。
Simlukafusp alfa(FAP-IL2v,RO6874281/RG7461)是一种免疫细胞因子,包含针对FAP的抗体和对IL-2Rβγ具有偏向性亲和力的IL-2变体。它被证明是一种有效的免疫细胞因子,在体外和体内增强了基于T细胞和NK细胞的不同癌症免疫疗法的疗效。
另一种策略是靶向CAF的下游效应器和/或信号通路,包括CAF衍生的细胞因子和趋化因子。例如,针对IL-6、IL-6R和IL-6下游JAK/STAT3信号通路的药物已被FDA批准用于骨髓增生性疾病和自身免疫性疾病,以抑制FAP+CAF诱导促炎细胞因子和促血管生成因子,它们增加癌细胞增殖和转移,并负性调节T细胞和NK细胞毒性活性。
除IL-6外,靶向TGF-β信号的治疗剂还可以干扰CAF的激活或减少CAF的数量,从而抑制肿瘤生长并具有抗肿瘤作用。Galunisertib是一种TGF-βRI激酶抑制剂,可特异性下调SMAD2的磷酸化,从而消除经典途径的激活。其已经对胶质母细胞瘤、肝细胞癌和胰腺癌患者进行了研究。
此外,靶向CAF还可以将促肿瘤性CAF的激活状态恢复为相对静止状态或肿瘤抑制表型。维生素D治疗可诱导基质重编程,使CAF活化表型正常化,抑制炎症和纤维化,提高化疗药物的摄取和胰腺星状细胞的存活率。
近年来,越来越多的证据表明CAF在多种癌症的发生、发展、免疫抑制和耐药性中的参与和重要性。作为TME的关键组成部分,CAF与TME以及整个宿主密切相关,根据不同的环境表现出表型和功能异质性。目前CAF在肿瘤发生和治疗耐药性中的研究热点主要集中在亚组分析和功能研究上,这些研究依赖于CAF特异性标记物和分泌物,如IFN-γ和TGF-β,它们在不同癌症阶段以特定于环境的方式在不同水平表达。
现有结果表明,CAF导向的抗癌策略中使用的一些靶向标记物实际上是非特异性的,并且在癌细胞上也可以找到。此外,缺氧、酸性微环境和肿瘤血管异常仍然是在实践中需要同时克服的障碍。为此,需要更合理的体外和体内研究模型。从策略的角度来看,开发组合策略,不仅针对CAF和TME之间的相互作用,而且促进常规治疗效果,仍然是临床试验设计的主流方向。此外,还应注意组合药物的剂量和潜在发生率,以真正实现未来的个体化抗癌治疗。
参考文献:
1. Cancer-associated fibroblasts andresistance to anticancer therapies: status, mechanisms, and countermeasures. CancerCell Int. 2022; 22: 166.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#抗肿瘤治疗#
32
#肿瘤相关成纤维细胞#
66
学习了,谢谢分享
36
认真学习了
41
坚持学习
45
#肿瘤治疗#
54
#成纤维细胞#
37
#纤维细胞#
40