JCEM:MAFLD与糖尿病、慢性肾病和心血管疾病的关联
2021-09-13 MedSci原创 MedSci原创
从NAFLD到MAFLD的变化对其与糖尿病、CKD和CVD之间的关联没有太大影响。采用MAFLD定义进一步确定了代谢性脂肪肝合并过度饮酒和HBV感染的患者,与非脂肪肝患者相比,发生糖尿病的风险增加。
2020年,代谢功能障碍相关脂肪肝(MAFLD)这一术语被提出来,并取代非酒精性脂肪肝(NAFLD)。近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,该研究旨在调查MAFLD的患病率和发病率,并评估其对肝外疾病的影响。

该研究共纳入了6873名受试者,随访时间为4.6年。研究人员使用Logistic回归和Cox比例风险模型评估MAFLD和NAFLD与糖尿病、慢性肾病(CKD)和心血管疾病(CVD)之间的关联。
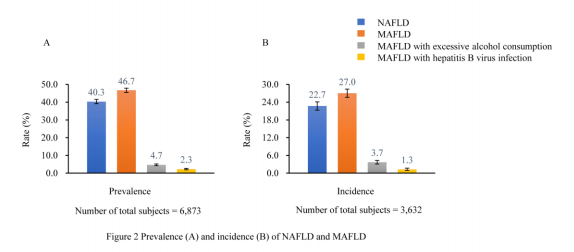
NAFLD和MAFLD的患病率分别为40.3%(95%置信区间[CI]为39.2-41.5)和46.7%(95%CI为45.6-47.9)。此外,321名(4.7%)和156名(2.3%)MAFLD受试者伴有过量饮酒和乙型肝炎病毒(HBV)感染。随访期间,NAFLD和MAFLD的发生率分别为22.7%(95%CI为21.3-24.0)和27.0%(95%CI为25.5-28.4)。
MAFLD与较高的糖尿病(风险比[RR]为2.08,95%CI为1.72-2.52)、CKD(RR为1.64,95%CI为1.39-1.94)和心血管疾病(风险比1.44,95%CI为1.15-1.81)发生风险相关。此外,在NAFLD患者中也观察到了类似的关联。此外,过量饮酒(RR为2.49,95%CI为1.64-3.78)和HBV感染(RR为1.98,95%CI为1.11-3.52)的MAFLD亚组与较高的糖尿病发病风险相关。
由此可见,从NAFLD到MAFLD的变化对其与糖尿病、CKD和CVD之间的关联没有太大影响。采用MAFLD定义进一步确定了代谢性脂肪肝合并过度饮酒和HBV感染的患者,与非脂肪肝患者相比,发生糖尿病的风险增加。
原始出处:
Yebei Liang.et al.Association of MAFLD with diabetes, chronic kidney disease, and cardiovascular disease: a 4.6-year cohort study in China.JCEM.2021.https://doi.org/10.1210/clinem/dgab641
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JCEM#
33
#AFLD#
34
#JCE#
39
#MAFLD#
27
#血管疾病#
33
代谢功能障碍相关脂肪肝
62
学习一下
63
把
63
谢谢MedSci提供最新的资讯
0