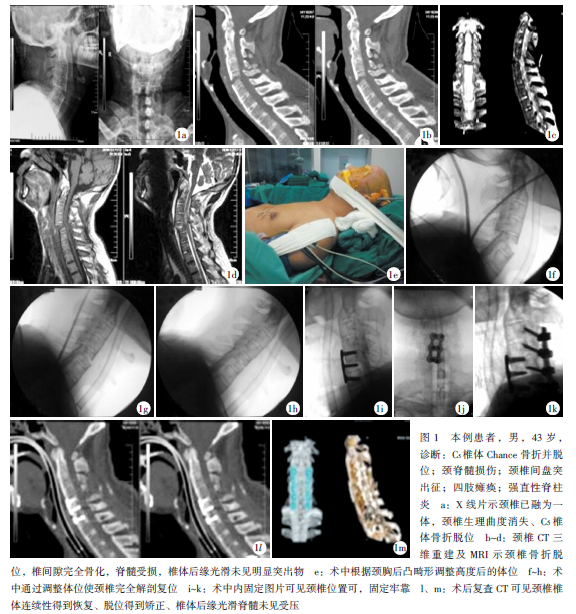
强直性脊柱炎并颈椎Chance骨折1例
2019-12-02 席金涛 徐峰 康辉 中国矫形外科杂志
患者,男,43岁,强直性脊柱炎病史20余年,现已稳定处于僵直期。因外伤致颈椎及四肢活动受限2d入院。患者自诉2018年2月6日醉酒后摔伤致颈部疼痛,四肢活动受限,感觉麻木,二便失禁,后被送当地医院行颈胸椎MRI扫描:(1)C5椎体骨折并滑脱(Ⅱ度),C4/5椎体水平脊髓损伤;(2)颈椎椎体及附件周围、胸廓周围入口处软组织弥漫性肿胀,颈椎前方积液;(3)颈胸段椎体强直性脊柱炎改变;颈椎X线片:C5椎
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












老师您好,患者出现肺部感染没有?有没有气管切开?谢谢
52
#强直性#
43
#颈椎Chance骨折#
32
#脊柱炎#
50
#CHANCE#
37
#CHANCE#
36