下颌智齿拔除致慢性中央型下颌骨骨髓炎1例
2018-10-20 侯雪莹 万阔 罗顺云 口腔医学
智齿拔除术是牙槽外科最常见的手术之一,80%的成年人都存在需要拔除的阻生智齿。智齿拔除术后并发症发生率总体为7%~10%,下颌发生率高于上颌,多为术后疼痛、肿胀、出血、神经损伤等,而术后感染的发生率为1%~15%。随着拔牙步骤的规范化,抗生素的应用以及患者人群口腔卫生的不断提高,拔牙创面合并感染偶有发生,干槽症发生率国外报道为0.5%~64.8%,国内报道为4%~10%,而感染发展成颌骨骨髓炎更为
智齿拔除术是牙槽外科最常见的手术之一,80%的成年人都存在需要拔除的阻生智齿。智齿拔除术后并发症发生率总体为7%~10%,下颌发生率高于上颌,多为术后疼痛、肿胀、出血、神经损伤等,而术后感染的发生率为1%~15%。随着拔牙步骤的规范化,抗生素的应用以及患者人群口腔卫生的不断提高,拔牙创面合并感染偶有发生,干槽症发生率国外报道为0.5%~64.8%,国内报道为4%~10%,而感染发展成颌骨骨髓炎更为罕见。希望通过本文报道的下颌智齿拔除引发慢性中央型下颌骨骨髓炎的病例讨论,引起广大临床医师的重视,并警惕拔牙术相关因素可能对颌骨骨髓炎发生的影响,同时对慢性中央型下颌骨骨髓炎有更全面的了解,预防此并发症的发生。
患者女,45岁,2013年3月以“右侧颌面部肿痛1周”求治于我院。患者5个月前于我院拔除右下阻生智齿,手术顺利,术前无反复冠周炎史,术后7d拆线无不适。4个月前自觉右侧颌下区隐痛不适,于外院冲洗取出一米粒大小骨片,后疼痛消失无不适。1周前无意间外力碰触右侧颌面部后觉该区疼痛不适,前来就诊。患者无系统性疾病及过敏史。专科检查见右侧下颌骨体及下颌角区轻度肿大,皮肤色泽基本正常无破溃,触痛不明显,双侧耳前、下颌及颈部未触及肿大淋巴结,开口度正常。
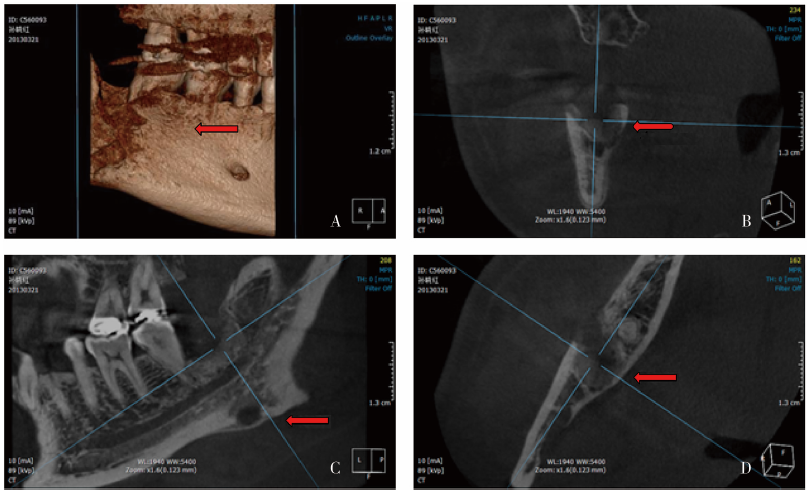
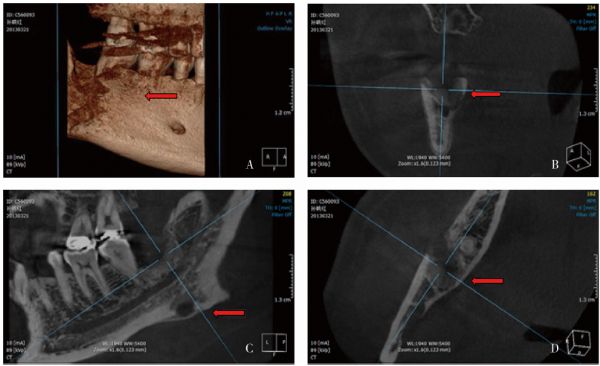
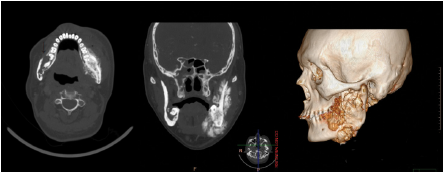
口内肿胀不明显,右下智齿拔牙创牙龈黏膜愈合良好,47牙冠完整,无叩痛,Ⅰ度松动,远中牙周袋8~10mm,牙周无溢脓。CBCT三维重建示48拔牙创未愈,周围骨组织呈隧道状破坏延伸至47远中及根端,达下颌骨体下缘(图1A);冠状位示48拔牙窝团块状死骨,周围骨质破坏,舌侧皮质骨近乎穿透(图1B);矢状位示48拔牙窝及周围骨质破坏,下颌角下缘可见层状骨膜反应(图1C);轴位示48拔牙窝周围松质骨破坏,颊侧皮质骨菲薄,舌侧皮质骨已穿通(图1D)。
图1 术前CBCT。A:三维立体重建示拔牙创未愈,骨组织呈隧道状破坏;B:冠状位示死骨形成,舌侧皮质骨近乎穿透;C:矢状位示骨膜反应;D:轴位示拔牙窝周围松质骨破坏,颊侧皮质骨菲薄呈线状
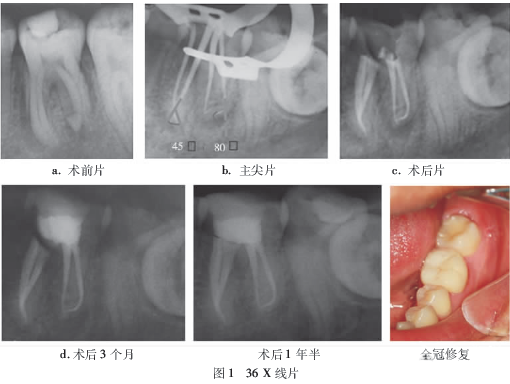
诊断:拔牙术后慢性中央型下颌骨骨髓炎,行“全麻下右下颌骨病灶探查搔刮术+47拔除术”,彻底搔刮死骨病灶,拔除远中及根尖骨质缺损的47,大量生理盐水冲洗,对位缝合,抗感染治疗5d。术后7d拆线创口愈合良好,病理结果显示为右下拔牙窝纤维结缔组织呈急性及慢性炎症,肉芽组织形成,可见少量骨组织。术后半年下颌骨痊愈,X线片检查47、48处颌骨密度略低于正常骨密度,颌骨病灶区基本恢复正常(图2),随访2年无复发。
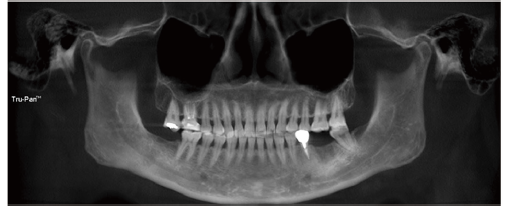
图2 术后6个月全口曲面断层片,图中示47、48处颌骨组织愈合
原始出处:
侯雪莹, 万阔, 罗顺云,等. 下颌智齿拔除致慢性中央型下颌骨骨髓炎1例[J]. 口腔医学, 2017, 37(4):361-363.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#下颌#
30
#中央型#
44
值得学习,这种情况是否可以避免
82
#骨髓炎#
38
#下颌骨#
30
#智齿#
30