European Radiology:CT扫描后儿童癌症风险的评估
2022-06-18 shaosai MedSci原创
在英国(UK)、澳大利亚、台湾、德国和荷兰,都有关于儿童时期接触CT扫描而导致中枢神经系统(CNS)肿瘤风险明显增加的报道。
 众所周知,计算机断层扫描(CT)提供的电离辐射(IR)剂量比传统的X射线程序要高[。然而,由于儿童对癌症部位有更高的辐射敏感性,以及更长的预期寿命,因此人们对儿童可能的癌症风险提出了担忧。在英国(UK)、澳大利亚、台湾、德国和荷兰,都有关于儿童时期接触CT扫描而导致中枢神经系统(CNS)肿瘤风险明显增加的报道。此外,一些研究指出,白血病的发病率与CT扫描暴露之间存在统计学上显著的正相关。
众所周知,计算机断层扫描(CT)提供的电离辐射(IR)剂量比传统的X射线程序要高[。然而,由于儿童对癌症部位有更高的辐射敏感性,以及更长的预期寿命,因此人们对儿童可能的癌症风险提出了担忧。在英国(UK)、澳大利亚、台湾、德国和荷兰,都有关于儿童时期接触CT扫描而导致中枢神经系统(CNS)肿瘤风险明显增加的报道。此外,一些研究指出,白血病的发病率与CT扫描暴露之间存在统计学上显著的正相关。
近日,发表在European Radiology杂志的一项研究根据改进的剂量估计,对一项来自法国的CT队列进行了长期随访,并提出中枢神经系统肿瘤、白血病和淋巴瘤的最新风险估计。
本研究对纳入患者从第一次做CT的日期(2000年至2011年之间)开始随访,死亡日期、首次癌症诊断日期或18岁生日日期。癌症发病率、生命状态、癌症诱发因素(PFs)和额外的CT扫描是通过外部国家数据库收集的。与累积器官剂量和性别相关的危险比(HRs)通过Cox模型进行评估。
在随访结束时,脑组织和红骨髓(RBM)的平均累积剂量分别为27.7和10.3 mGy。在没有PFs的患者中,估计中枢神经系统肿瘤每10mGy的HR为1.05(95%CI:1.01-1.09),白血病为1.17(95%CI:1.09-1.26),淋巴瘤为0.96(95%CI:0.63-1.45)。这些估计值没有因为纳入参与医院之外或纳入期之后进行的CT扫描而改变。
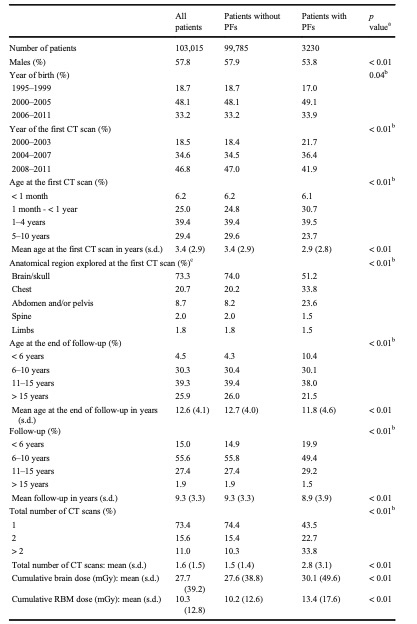
表 在最新的法国CT队列中,患者的特征和CT扫描暴露与是否存在易致癌的临床因素(PFs)有关
本研究显示,对于没有癌症PFs的患者,随着吸收剂量的增加,CT相关的辐射照射会产生小的统计学意义上的中枢神经系统肿瘤和白血病风险的增加。然而,对于有PFs的患者,没有观察到相关的证据。此外,HR估计值没有受到纳入SNDS中收集的、在纳入期间或之后在参与医院之外进行的CT扫描的影响。
原文出处:
Anaïs Foucault,Sophie Ancelet,Serge Dreuil,et al.Childhood cancer risks estimates following CT scans: an update of the French CT cohort study.DOI:10.1007/s00330-022-08602-z
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
42
学习了
42
#儿童癌症#
54
#CT扫描#
44
😯学习。。。
41