Pediatrics:儿童探视中常规体温测量的频率和结果
2022-01-26 从医路漫漫 MedSci原创
健康儿童就诊是儿童接受非卧床看护的最常见原因。美国儿科学会预防护理指南“光明未来”就健康监督、预见性指导、疾病和发育筛查提供建议,对从出生到青春期的健康儿童就诊。
背景:健康儿童就诊是儿童接受非卧床看护的最常见原因。美国儿科学会预防护理指南“光明未来”就健康监督、预见性指导、疾病和发育筛查提供建议,对从出生到青春期的健康儿童就诊。它建议在出生一年内就诊7次,1-3岁就诊5次,然后每年至青春期就诊5次。虽然对其他生命体征提出了建议,但体温测量并不包括在指南内。
我们之前的研究使用公开的全国性调查数据(全国非卧床医疗护理调查),报告说体温测量几乎占所有健康儿童就诊人数的一半。在健康儿童就诊时,常规测量在无症状儿童中的效用尚未确定,可能会产生不良后果,如降低临床效率、患者焦虑和“发烧恐惧症”(定义为对发烧危害的夸大担忧)的放大。此外,通过常规测量偶然发现体温升高可能会导致“过度诊断”。我们发现,在测量体温的就诊中,抗生素和X光片的使用频率更高,即使在没有发烧的情况下也是如此。由于这些数据的局限性,我们无法确定临床方案和患者症状是否有助于体温测量。
目的:确定(1)常规体温测量的频度和就诊特点,(2)体温测量的干预率和偶然发现发热的概率。
方法:在这项回顾性队列研究中,我们分析了2014-2019年间健康儿童的访问情况。我们进行了多变量回归来表征与常规体温测量相关的就诊情况,并进行了广义估计方程回归,以根据体温测量和发热状态来确定干预措施(抗生素处方和诊断测试)和疫苗延期的调整率,并按临床和患者进行分组。通过双重独立的图表检查,发烧(≥100.4°F)被分类为可能、不太可能被偶然检测到。
结果:274351例(58.9%)健康儿童就诊中,体温测量发生在155527例(58.9%)。在24个门诊中,16个门诊(常规测量诊所)的体温测量大于90%,8个门诊(“不定期测量诊所”)的体温测量<20%。在调整了年龄、种族、种族和保险后,抗生素处方更常见(调整后的优势比:1.21;95%可信区间为1.13-1.29),而诊断性测试在常规测量诊所较不常见(调整后的优势比:0.76;95%可信区间为0.71-0.82)。在155527人次的常规测量门诊中,有270人次(0.2%)检出发热,其中47人次(17.4%)被归类为可能的偶发发热。抗生素处方和诊断测试在可能有偶发发烧的就诊中比无发烧就诊时更常见(7.4%比1.7%;14.8%比1.2%;P<0.001),疫苗接种推迟了50%。
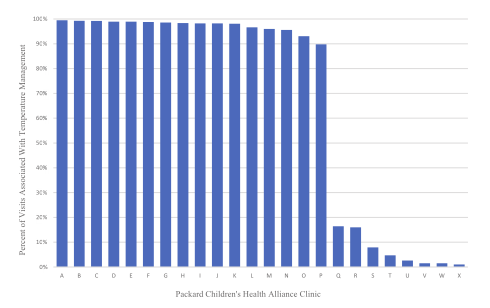
图 健康儿童就诊时体温测量的百分比,由诊所提供。
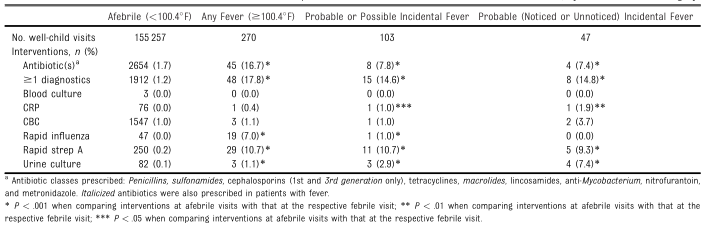
表1 按偶发发热类别划分的在常规测量诊所测量体温的儿童就诊中的干预率
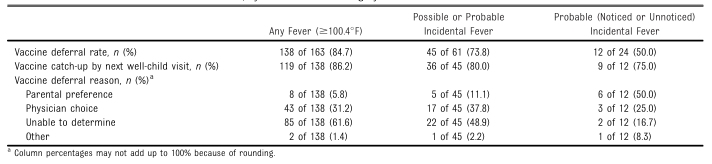
表2 按偶发发热类别划分的发热就诊延迟接种比率
结论:体温测量是在一半以上的健康儿童就诊时进行的,是一种诊所常有的做法。考虑到对后续干预和疫苗延期的影响,这种做法的危害-益处概况值得考虑。
原文出处:Dang R, Patel AI, Marlow J,et al.Frequency and Consequences of Routine Temperature Measurement at Well-Child Visits.Pediatrics 2021 Dec 13
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Pediatric#
41
#PE#
46
#DIA#
33
学习
35
学习
58