Hypertension:高血压和降压药治疗对COVID-19住院患者死亡率的影响
2022-09-16 MedSci原创 MedSci原创
尽管既往高血压的诊断本身对COVID-19患者的住院死亡率没有显著影响,但任何一线降压药的治疗对高血压患者的生存都有显著的益处。这些数据支持在COVID-19大流行期间坚持降压药物治疗的必要性。
高血压等心血管疾病是新冠肺炎住院患者的常见合并症。近日,心血管权威杂志Hypertension上发表了一篇研究文章,研究人员旨在评估既往有高血压及其药物治疗对COVID-19住院患者住院死亡率的影响。
研究人员分析了2020年3月至2021年5月期间因COVID-19住院的波兰克拉科夫大学医院的所有连续就诊的患者。此外,研究人员分析了5191例患者(平均年龄为61.9±16.7岁,45.2%女性)的资料。
受试者中位住院时间为14天,死亡率为18.4%。约四分之一的患者伴有心血管疾病,包括冠状动脉疾病(16.6%)或卒中(7.6%)。高血压患者(58.3%)年龄较大,合并症多于无高血压患者。
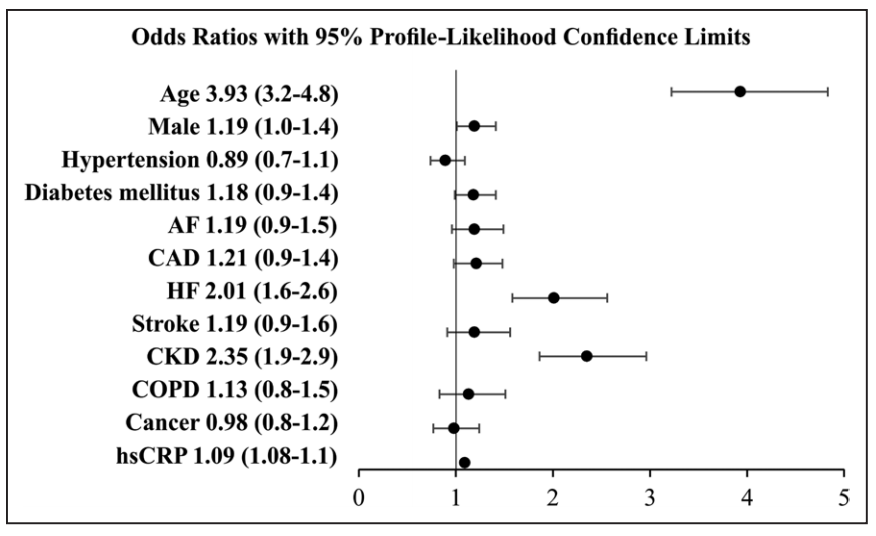
在多变量logistic回归分析中,年龄在中位(64岁)以上、男性、心力衰竭或慢性肾脏病史、c反应蛋白水平较高是住院死亡的独立危险因素。与未接受治疗的高血压相比(n=1305),已经接受过任何一线降压药(血管紧张素转换酶抑制剂、血管紧张素受体阻滞剂、β-阻滞剂、钙通道阻滞剂或噻嗪类利尿剂)治疗的高血压患者(n=1723)住院死亡的风险显著降低(比值比为0.25[95%CI为0.2-0.3];P<0.001)。
由此可见,尽管既往高血压的诊断本身对COVID-19患者的住院死亡率没有显著影响,但任何一线降压药的治疗对高血压患者的生存都有显著的益处。这些数据支持在COVID-19大流行期间坚持降压药物治疗的必要性。
原始出处:
Wiktoria Wojciechowska.et al.Impact of Arterial Hypertension and Use of Antihypertensive Pharmacotherapy on Mortality in Patients Hospitalized due to COVID-19: The CRACoV-HHS Study.Hypertension.2022.https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.122.19575
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
51
#患者死亡#
50
#TENS#
57
#降压#
77
#Hypertension#
64