JCEM:胸椎骨折在COVID-19患者中常见且可预测疾病预后
2020-10-22 MedSci原创 MedSci原创
VFs可能整合了COVID-19患者的心肺风险,是一种有用且易于测量脆弱性和不良预后的临床指标。研究人员建议应对所有接受胸部X线检查的可疑COVID-19患者进行胸椎形态学评估。
COVID-19已成为全球最受关注的医学问题。尽管有几项研究调查了COVID-19患者的临床特征,但尚未有研究报道椎骨骨折(VFs)患病率的数据。VF可能会影响心肺功能和疾病结局,近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,该研究旨在评估VF的患病率和对COVID-19患者临床结局的影响。
这是一项在意大利三级医疗医院进行的回顾性队列研究,研究人员纳入了到急诊科就诊且接受侧位胸部X光检查的COVID-19患者。研究人员通过胸部X射线对椎体形状进行半定量评估来检测有无VF。
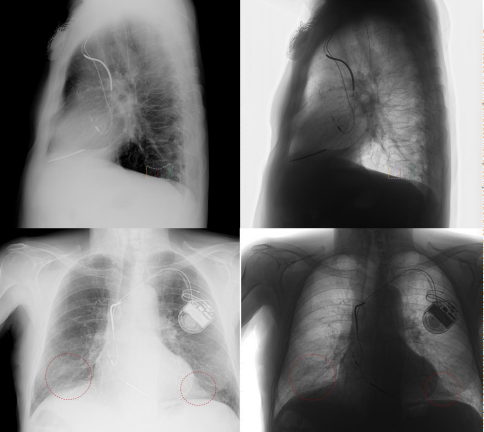
该研究共纳入了114例患者,其中41例(36%)检测出存在胸VF。VF患者年龄较大,并且更容易受到高血压和冠状动脉疾病的影响(分别为p<0.001,p=0.007,p=0.034)。
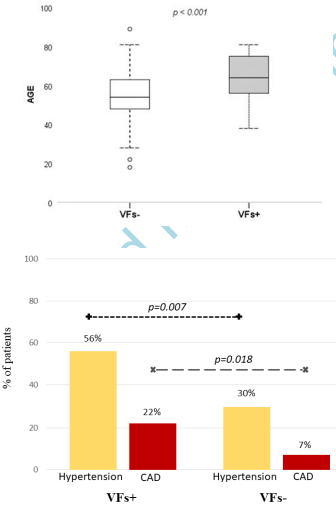
VFs组有36例(88%)患者入院,而无VFs组有54例(74%)患者入院(p=0.08)。与没有VF的患者相比,有VF的患者更需要无创机械通气(p=0.02)。VFs组的死亡率为22%,无VFs组的死亡率为10%(p=0.07)。特别是重度VF患者的死亡率高于中度和轻度VF患者(p=0.04)。
由此可见,VFs可能整合了COVID-19患者的心肺风险,是一种有用且易于测量脆弱性和不良预后的临床指标。研究人员建议应对所有接受胸部X线检查的可疑COVID-19患者进行胸椎形态学评估。
原始出处:
Luigi di Filippo,et al.Radiological Thoracic Vertebral Fractures are highly prevalent in COVID-19 and predict disease outcomes.JCEM.2020.https://doi.org/10.1210/clinem/dgaa738
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#JCE#
23
#JCEM#
26
#疾病预后#
34
#COVID-19患者#
20
#胸椎#
38