Cell Rep: 肠道细菌或能通过刺激免疫细胞对抗结直肠癌
2020-04-12 竹子 转化医学网
来自法国Collège大学微生物系的一项研究证明,肠道菌群失衡会促进结直肠癌的发作。
我们肠道中的微生物,是个神奇的“黑匣子”,它们可以和我们所吃的食物直接接触,对下游的健康产生影响。随着肠道微生物研究的“崛起”,陆续有研究人员发现,结直肠癌的发生发展也和它有一些联系。来自法国Collège大学微生物系的一项研究证明,肠道菌群失衡会促进结直肠癌的发作。促进伤口愈合的免疫细胞与肿瘤恶化息息相关,并且它们还会促进肿瘤生长,而肠道微生物可以刺激免疫系统对抗癌症。目前,研究人员们通过免疫细胞这个切口对胃肠道中的微生物如何影响结直肠癌的发展进行了研究。
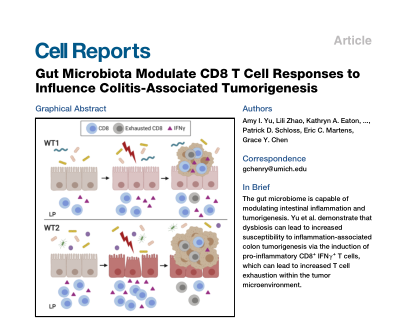
近日,美国密歇根大学罗杰尔癌症中心的研究人员将研究结果发表在Cell子刊《Cell Reports》上。他们发现,某些类型的肠道细菌在刺激体内某些免疫细胞(特别是CD8 + T细胞)方面要优于其他类型。虽然这些细胞毒性T细胞(CD8 + T细胞)通常有利于保护人体对抗癌症,但过度刺激会导致炎症和T细胞耗尽,这实际上增加了其对癌症的易感性。这项工作将帮助科学家查明哪些细菌能抑制或促进肿瘤生长。
根据美国癌症协会的统计,在美国,结直肠癌(CRC)是全世界第三大常见癌症原因,也是第四大癌症相关死亡原因。
密歇根医学大学血液学肿瘤学副教授,罗杰尔癌症中心的成员资深研究作者Grace Chen医学博士说:“人们对细菌在提高免疫疗法有效性中的作用也感到非常兴奋。这项工作表明它可能是一把双刃剑,研究人员需要注意其导致T细胞耗尽。”
不同的老鼠,不同的结果
当前的研究是建立在Chen研究小组以前的工作的基础上的,该研究发现肠道微生物组的紊乱可以直接促进癌症的发展。
该小组发现,来自两个不同群落的小鼠在接触致癌物以及导致胃肠道炎症的药物时,对结直肠癌的敏感性差异很大。
来自第一个群落的小鼠平均长五个肿瘤,而来自第二个群落的小鼠平均长15个肿瘤并炎症反应也更明显。
当研究人员对来自两个不同群落的粪便细菌进行测序时,他们发现它们具有由不同类型细菌组成的独特微生物群落。
Chen说:“这令人兴奋,哪种细菌对结肠直肠癌风险的影响最大,以及通过何种机制产生影响,这是我们实验室的关注点。”
相同的老鼠,不同的结果
为了更好地了解是什么导致了研究人员在两个不同实验室中观察到的差异,他们将两个群落中的每一个的肠道细菌移植到了在无菌环境中繁殖的基因相同的小鼠中。同样,第二个群落的小鼠表现更糟。
Yu说:“这表明不同的肠道菌群直接促进了肿瘤的发展。我们的数据最终揭示了九种不同的细菌种群,它们可能具有抑癌或促肿瘤活性。”
调查机制
接下来,为了更好地了解是什么导致了来自第二个小鼠群落的细菌增加的炎症和肿瘤生长,研究小组进行了实验。
通过免疫细胞分析,他们发现老鼠的结肠组织中有来自第二个群落的细菌,其中有更多的T细胞,还有更多的CD8 +细胞。
Chen说:“这有点反常,因为T细胞和CD8 +细胞通常在结直肠癌患者中具有更好的预后。我们假设这些细胞在某些细菌的存在下会过度活化,然后耗尽,使它们杀死肿瘤细胞的能力降低。”
Chen指出,当将第二个小鼠群落的细菌移植到经过设计的缺少CD8 + T细胞的小鼠中时,肿瘤的产生就会减少,从而支持T细胞在某些细菌存在下促进癌症生长的作用。
同时,实验室继续在研究的基础上研究各种细菌可能有助于促进或预防结直肠癌发展的机制。
原始出处:Amy I. Yu, Lili Zhao, Kathryn A. Eaton, et al. Gut Microbiota Modulate CD8 T Cell Responses to Influence Colitis-Associated Tumorigenesis. Cell Reports(2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












关注
55
#CEL#
33
#Cell#
32
#肠道细菌#
38
#结直肠#
30