Dig Dis Sci: 中度至重度溃疡性结肠炎患者尝试使用英夫利昔单抗时代表5-氨基水杨酸酯治疗就无效了
2020-11-22 MedSci原创 MedSci原创
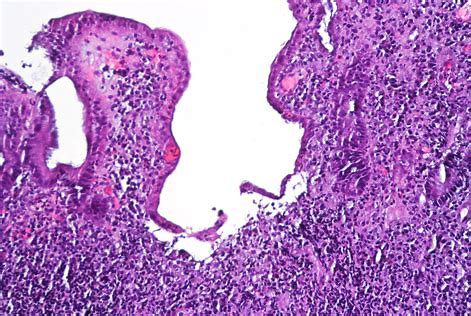
溃疡性结肠炎(UC)的特征是疾病活动和缓解交替发作,UC的治疗目标是通过在疾病早期引入高效治疗药物来诱导和维持疾病缓解以及预防并发症。
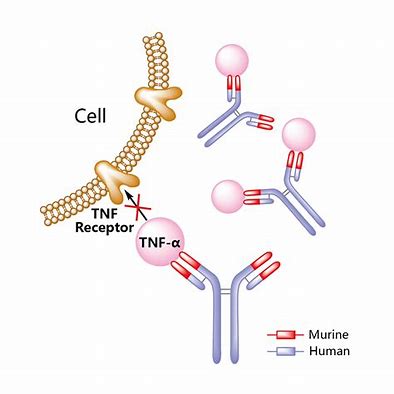
溃疡性结肠炎(UC)的特征是疾病活动和缓解交替发作,UC的治疗目标是通过在疾病早期引入高效治疗药物来诱导和维持疾病缓解以及预防并发症的发生,对于轻度至中度UC,目前的文献和指南支持使用5-氨基水杨酸(5-ASA)的一线治疗,以诱导和维持缓解,,但是尽管有5-ASA治疗,但仍有一部分患者进展为中度至重度UC,需要升级为生物制剂或小分子治疗。生物制剂:抗肿瘤坏死因子-α(抗TNF)治疗是在诱导和维持5-ASA疗法无效的患者中有强大疗效。然而,尚不清楚在升级为抗TNF治疗的患者中应停止还是继续使用5-ASA。因此,本项研究旨在评估伴随5-ASA治疗对逐步升级为英夫利昔单抗的溃疡性结肠炎(UC)患者临床结局的影响。
这是一项回顾性研究,研究人员回顾了2012年1月至2017年12月在阿尔伯塔大学开始使用英夫利昔单抗治疗的中度至重度UC患者的临床情况。主要观察结果是在6和12个月时临床缓解(部分Mayo评分<2)程度。次要观察结果包括内窥镜检查(内镜Mayo <2)和深度缓解(临床和内窥镜检查合并缓解),住院或结肠切除术。单因素和多元逻辑回归模型用于估计结果的优势比和95%CI。
研究人员在47个月的平均随访时间内随访了112位患者。使用5-ASA的患者同时使用免疫调节剂的比例增加(73.3% VS 54.1%,p = 0.03)。在6个月(aOR 2.59,p = 0.07)或12个月(aOR 0.43,p = 0.06)时临床缓解率无差异。在12个月时,同时接受5-ASA的患者不太可能实现内窥镜下缓解(aOR 0.08,p = 0.01)和深度缓解(aOR 0.07,p = 0.02)。两组之间的不良结局(如需要急救治疗,住院和结肠切除术)没有差异。

因此,通过本项研究证实了已经升级为英夫利昔单抗治疗的中重度UC患者可以停止5-ASA,因为它没有控制炎症的额外益处。
原始出处:
Bhairavi Balram. Et al. Concomitant 5-Aminosalicylate Therapy in Moderate-to-Severe Ulcerative Colitis Patients Escalated to Infliximab Is Not Beneficial. Digestive Diseases and Sciences.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#水杨酸#
34
#中度至重度#
37
#溃疡性#
35
#Dis#
29