不同类型流产的超声表现
2020-08-16 即时超声 即时超声
发生在12周以前的流产定义为早期流产,妊娠12周至不足28周的流产定义为晚期流产。据估计,在人类全部妊娠中,约75%以自然流产告终。
发生在12周以前的流产定义为早期流产,妊娠12周至不足28周的流产定义为晚期流产。据估计,在人类全部妊娠中,约75%以自然流产告终。其中,大部分胚胎在着床后很快就停止发育,仅表现为月经过多或月经延期,即早早孕流产。
80%以上的流产发生在妊娠12周以内,随后流产率迅速下降。至少半数以上早期流产是由胚胎染色体异常所致。自然流产风险随产次、父母年龄增加而升高。常见流产原因包括:
1.染色体异常
包括夫妻染色体异常和胚胎染色体异常。常见的夫妇染色体异常为平衡易位、罗伯逊易位等。胚胎染色体异常中三倍体最多、其次为多倍体、X单体、常染色体单体、染色体平衡易位、缺失、嵌合体、倒置、重叠等。复发性流产夫妇染色体异常的发生率为4%,而正常人群为0.2%,其中母源与父源之比为3:1。单次自然流产中胚胎染色体异常为主要原因,随流产次数的增加胚胎染色体异常发生率减少。
2.母体内分泌失调
(1)黄体功能不全 占23%~60%,基础体温双相型,但高温相小于11日,或高低温差小于0.3℃,子宫内膜活检示分泌反应至少落后2日,黄体期孕酮低于15ng/ml引起妊娠蜕膜反应不良,2~3个周期黄体功能检测显示不足,方可纳入诊断,黄体功能不全影响孕卵着床。
(2)多囊卵巢综合征 高浓度的促黄体生成素,高雄激素和高胰岛素血症降低了卵子质量和子宫内膜容受性,容易导致流产发生。
(3)高泌乳素血症 黄体细胞存在泌乳素受体,高泌乳素抑制颗粒细胞黄素化及类固醇激素,导致黄体功能不全和卵子质量下降。
(4)甲状腺疾病 甲状腺功能低下与反复发生的自然流产相关。
(5)糖尿病 亚临床或控制满意的糖尿病不会导致流产,未经控制的胰岛素依赖型糖尿病自然流产率增加。
3.母体生殖道的异常
(1)子宫畸形 包括单角子宫、双角子宫、双子宫及子宫纵隔等。其中尤以子宫不全纵隔最易导致流产及早产。主要由于纵隔部位内膜发育不良,对甾体激素不敏感,血液供应差。
(2)Asherman综合征 宫腔体积缩小,对甾体激素应答下降。
(3)宫颈机能不全 引起晚期流产和早产,是导致妊娠中期流产的主要原因。
(4)子宫肌瘤 黏膜下肌瘤及大于5cm肌间肌瘤的与流产有关。
4.生殖道感染
细菌性阴道病患者妊娠晚期流产及早产发生率升高,沙眼衣原体、解脲支原体造成子宫内膜炎或宫颈管炎可致流产。
5.其他
不健康生活方式与流产相关。有学者报道,每天吸烟超过14支的女性,流产风险较对照组增加2倍。酗酒、过量饮用咖啡因以及环境因素如有机溶剂和毒物等的影响。
临床上流产可分为先兆流产、难免流产、不全流产和完全流产四个阶段,另外还有胚胎停止发育较长时间仍未排出的过期流产(稽留流产)。临床表现与超声图像在各类型均有不同的特点。
一、先兆流产
临床表现:少量阴道流血或轻微下腹痛,宫口未开,胎膜完整、胚胎存活,子宫大小与孕周相符,妊娠试验阳性。此期可行安胎治疗。
二维声像:宫内妊娠囊内见胚胎或胎儿,大小符合孕周,有胎心搏动,胚囊与子宫壁之间见云雾状暗区,为绒毛膜从宫壁剥离、局部积血,见图1。当剥离范围进行性增大时,胚胎停止发育,转变为难免流产。
彩超表现:妊娠8周前的胚胎原始心管搏动约为70~80次/分,8周以后大于120次/分,若低于85次/分则有流产倾向;胎心搏动呈闪烁血流信号,见图2,血流频谱无舒张期成分,高回声的绒毛膜下仍有低阻力的滋养层血流。

图1 先兆流产绒毛膜下血肿声像
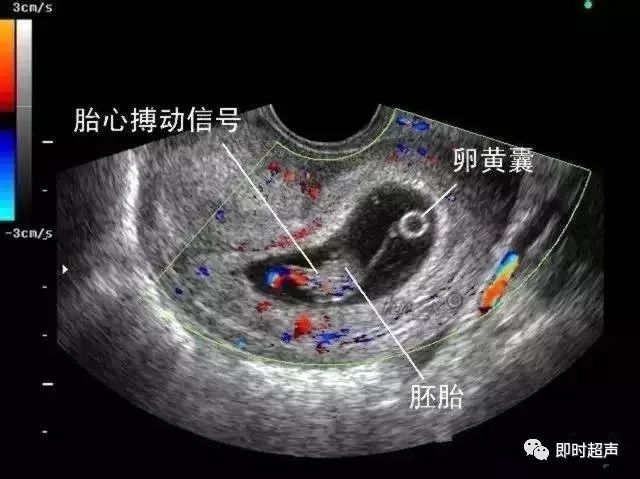
图2 先兆流产彩超表现
二、难免流产
临床表现:流产已不可避免,阴道流血量增多或出现阴道流水,腹痛加剧。宫颈口已开,孕囊下移。
二维声像:孕囊变形,下移至子宫下段或宫颈管内,甚至排出至宫颈外口或阴道内,胚胎常死亡,胚胎形态可辨,可见绒毛膜剥离征象,或宫腔积血声像,见图3。
彩超表现:妊娠囊内无胎心搏动信号,若孕囊未剥离,则仍可记录到低阻力的滋养层血流。若孕囊下移至宫颈管内,与宫颈部位的异位妊娠鉴别可以通过观察局部宫颈肌层有无局灶性扩张的血管,若血流丰富,应考虑宫颈妊娠。

图3 难免流产孕囊下移至宫颈管声像
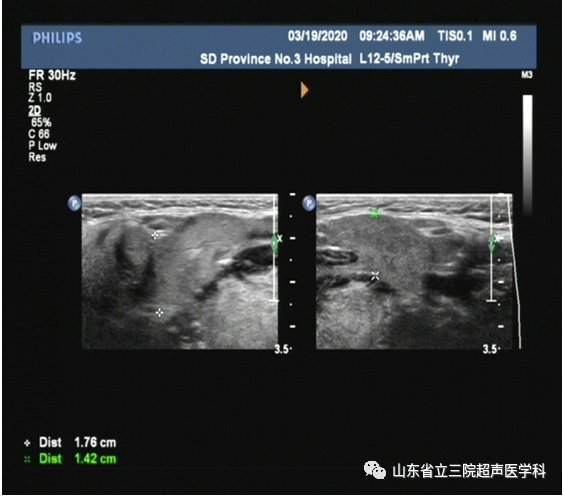
三、稽留流产
临床表现:胚胎或胎儿已死亡未及时排出而长时间存在子宫腔内。多数胚胎已枯萎,可有先兆流产症状,如少量阴道流血。子宫颈口关闭,子宫小于相应孕周。
二维声像:子宫小于相应停经孕周,宫腔内可见孕囊变形、不规则,囊内无正常胚胎,残存的胚胎呈一高回声团,位于囊内一侧,有时妊娠囊不清,仅残存胎盘绒毛,并宫腔积液,见图4。部分胎盘可发生水肿变性(胎盘部分水泡样变),呈大小不等的蜂窝状液性暗区,见图4-1-5,可根据血、尿HCG水平与葡萄胎鉴别。
彩超表现:妊娠囊内无胎心搏动信号,仍可记录到低阻力的滋养层血流频谱。
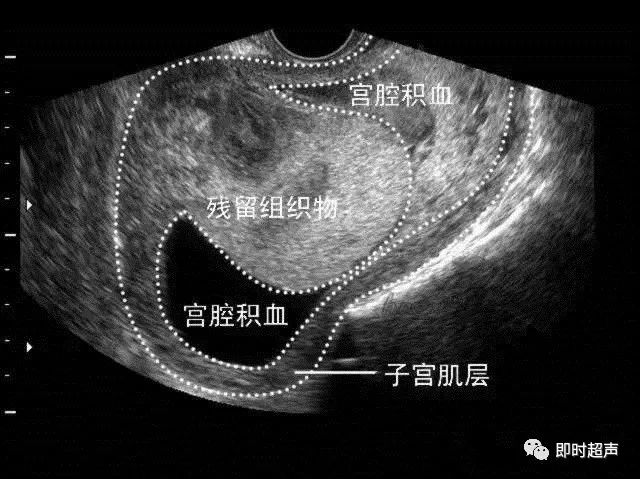
图4 稽留流产声像

图5 稽留流产胎盘水泡样变
四、不全流产
临床表现:妊娠囊已排出,宫腔内仍残留部分组织物及血块,阴道出血较多,宫颈口可见活动性出血或组织物堵塞,子宫小于相应孕周。组织物残留少时出血不会太多。如果组织物残留时间过长,可合并感染,临床上多有发热、白细胞增多等表现,为感染性流产。
二维声像:子宫比相应孕周小,宫腔内见不规则斑状、团状高回声,或见少许液性暗区。不均质高回声的大小根据组织物及血块的多少而不同。
彩超表现:子宫腔内不均质高回声内无血流信号,但相邻局部肌层内可见丰富的血流信号,可记录到低阻力型的类滋养层周围血流频谱。对于宫腔内少量组织物残留有无绒毛组织残留的判断,彩超起到重要的作用。
五、完全流产
临床表现:妊娠组织物已完全排出,阴道流血减少,宫颈口闭合,子宫恢复正常大小。
超声表现:子宫大小接近正常,宫腔内膜已呈线状,宫腔内可有少许积血声像。
注意:超声诊断与临床诊断不同,大多数情况下,超声只能提示宫腔内有无孕囊、孕囊内有无胚胎、胚胎有无存活,描述孕囊有无变形、绒毛膜有无剥离等。一般不作流产的临床诊断。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习了
80
#超声表现#
36
学习了!
83
好
87
不错
106
#不同类型#
55
学习了
95
好
81
收了
73