JACC:PCI术后高出血风险患者诊断标准的验证
2020-06-03 MedSci原创 MedSci原创
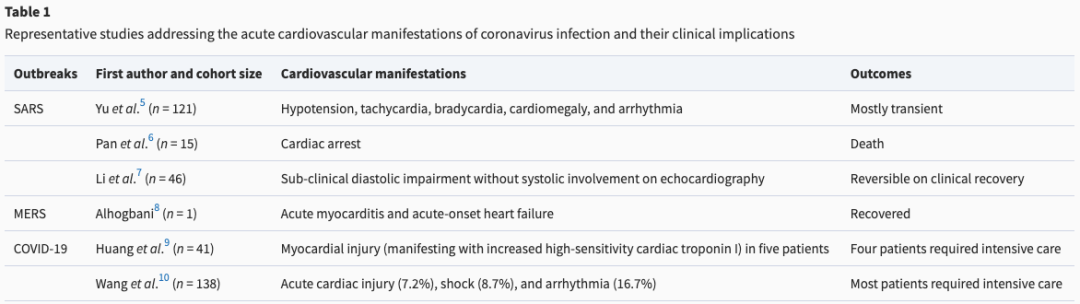
经皮冠状动脉介入治疗后出血具有重要的预后意义。学术研究联合会(ARC)最近提出了一系列临床标准来定义高出血风险(HBR)患者。本研究的目的旨在对ARC提出的HBR临床标准进行验证。
经皮冠状动脉介入治疗后出血具有重要的预后意义。学术研究联合会(ARC)最近提出了一系列临床标准来定义高出血风险(HBR)患者。本研究的目的旨在对ARC提出的HBR临床标准进行验证。
本研究纳入分析了9623名接受冠脉支架植入的患者,其中4278名(44.4%)被诊断为HBR患者。主要终点是1年时的院内或出院后出血。次要终点包括主要出血终点的个体成分、心肌梗死和全因死亡率。中重度的贫血是最常见的主要诊断标准(33.2%),年龄≥75岁是最常见的次要诊断标准。HBR患者1年的主要出血终点发生率为9.1%,而非HBR患者为3.2%(p<0.001),出血风险随着ARC-HBR定义完成次数的增加而逐步增加。HBR患者的所有次要终点的发生率也明显更高。
本研究结果在当代接受冠脉支架植入的患者中验证了ARC提出的诊断HBR的标准,ARC-HBR定义不仅确定了出血风险增加的患者,还确定了血栓事件风险增加的患者,包括全因死亡率。
原始出处:
Davide C et al.Validation of the Academic Research Consortium High Bleeding Risk Definition in Contemporary PCI Patients.JACC.2020 June.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PCI术#
39
好!!!!!
103
#JACC#
32
#ACC#
21
#诊断标准#
40
#PCI术后#
40
#高出血风险#
29