Eur Heart J:中性粒细胞-淋巴细胞比值与动脉粥样硬化事件的关系
2021-01-10 MedSci原创 MedSci原创
NLR是一种容易获得的炎症生物标志物,可独立预测CV风险和全因死亡率,可通过用卡那单抗阻断白介素-1β来降低NLR。
中性粒细胞-淋巴细胞比值(NLR)是一种很容易获得的炎症生物标志物,可能与动脉粥样硬化和心血管(CV)事件相关。近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,该研究旨在明确NLR是否能预测重大不良心血管事件(MACE)的发生,并是否可被抗炎治疗改善。

研究人员根据CANTOS、JUPITER、SPIRE-1、SPIRE-2和CIRT试验随机分配的60087名参与者的全血计数计算了基线和治疗期间的NLRs,这些研究的参与者分别接受安慰剂或卡那单抗、瑞舒伐他汀、bococizumab或甲氨喋呤,并随访至MACE。所有的分析都首先在CANTOS试验中进行,然后在其他四个试验中进行外部验证。在这5项试验中,研究人员使用Cox比例风险模型计算了主要CV事件的风险比,并比较了NLR四分位数患者的死亡率。
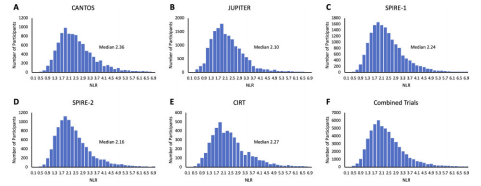
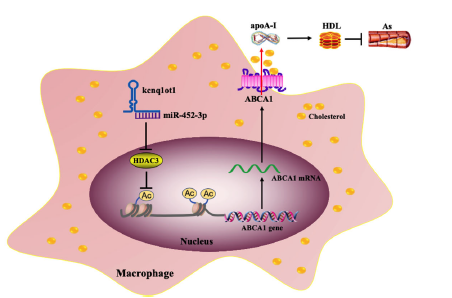
NLR与白细胞介素-6、c反应蛋白和纤维蛋白原水平轻度相关,但与脂质水平相关性最低。在所有5个随机试验中,基线NLR可预测CV事件和死亡;NLR四分位数增加在CANTOS试验中MACE风险是20%(95%可信区间(CI)为14 - 25%, P<0.0001], SPIRE-1试验中为31% (95%CI为14 - 49%, P=0.00007), SPIRE-2试验中为27% (95%CI为12 - 43%, P=0.0002), CIRT试验中为9% (95%CI为0.2 -20%, P=0.045),JUPITER试验中为11%(95%CI为1-22%,P=0.03)。降脂药物对NLR没有显著影响,采用卡那单抗进行抗炎治疗可降低NLR (P<0.0001)。
NLR是一种容易获得的炎症生物标志物,可独立预测CV风险和全因死亡率,可通过用卡那单抗阻断白介素-1β来降低NLR。
原始出处:
Nicholas H Adamstein,et al.The neutrophil–lymphocyte ratio and incident atherosclerotic events: analyses from five contemporary randomized trials.European Heart Journal.2021.https://doi.org/10.1093/eurheartj/ehaa1034
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#粥样硬化#
34
#中性粒细胞#
27
#淋巴细胞#
31
#ART#
25
#HEART#
31
#学习#动脉粥样硬化
101
好文辜!
92