JACC:对侧颈动脉闭塞对颈动脉血运重建术患者的预后影响
2021-03-03 Nebula MedSci原创
对侧颈动脉闭塞(CCO)的存在是接受颈动脉内膜切除术(CEA)的患者公认的高危特征,传统上也是颈动脉支架植入术(CAS)的适应症。最新观测数据令人质疑CCO是否仍是CEA的高危特征。
对侧颈动脉闭塞(CCO)的存在是接受颈动脉内膜切除术(CEA)的患者公认的高危特征,传统上也是颈动脉支架植入术(CAS)的适应症。最新观测数据令人质疑CCO是否仍是CEA的高危特征。
本研究的目的是在全国范围内明确CCO对接受CEA和CAS治疗的患者的临床预后的影响。
纳入了2007-2019年在NCDR CARE(国家心血管数据登记中心)和PVI(外周血管干预)登记的所有接受CEA或CAS治疗的患者。主要暴露是CCO的存在与否。评估指标是住院死亡、卒中和心肌梗死的综合结果。
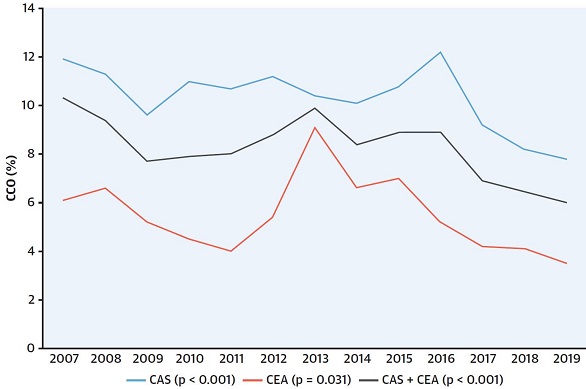
颈动脉血运重建术的患者的CCO发生率趋势
在58423例接受颈动脉血运重建术的患者中,4624例(7.9%)患者存在CCO。其中,68.9%(n=3185)的CCO患者接受了CAS治疗,31.1%(n=1439)的CCO患者接受了CEA治疗。
CCO患者平均69.5±9.7岁,女性占32.6%,白种人占92.8%,51.7%的有短暂性脑缺血发作或卒中史,45.4%的有症状性疾病。
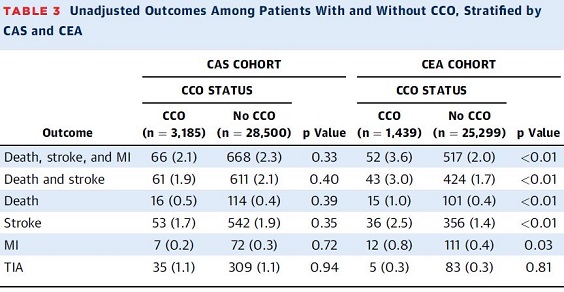
有无CCO患者的未调整预后
在研究期间,接受颈动脉血运重建术的患者的CCO患病率下降了41.7%(p<0.001),但CAS仍然是主要的血运重建策略。CAS后出现CCO的患者的未调整的综合结果的发生率(2.1%)低于CEA后出现CCO的患者(3.6%)。
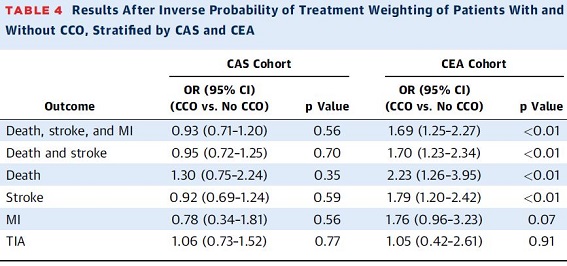
有无CCO患者的调整预后
调整后,CCO与CEA后不良结局几率增加71%(95%CI:1.2 7~2.30;P<0.001)相关,相比之下,CCO与CAS术后患者的综合结果发生率增加无关(调整后的优势比:0.94;95%CI:0.72~1.2 2;P=0.64)。
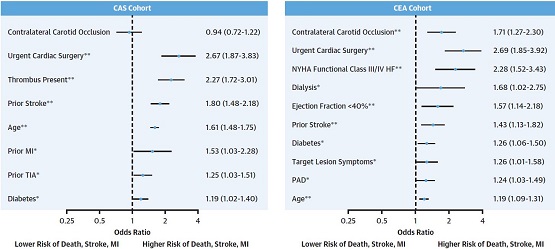
CAS或CEA失活患者院内事件风险增加的相关因素
总而言之,CCO仍然是接受CEA治疗的患者不良预后风险增加的重要预测因子,但与接受CAS治疗的患者的预后无关。
原始出处:
Krawisz Anna K,Rosenfield Kenneth,White Christopher J et al. Clinical Impact of Contralateral Carotid Occlusion in Patients Undergoing Carotid Artery Revascularization. J Am Coll Cardiol, 2021, 77: 835-844.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#血运重建术#
40
#JACC#
32
#颈动脉#
37
#动脉血#
44
#动脉闭塞#
53
已读,受益匪浅
87
#ACC#
33
临床正好碰到这样的难题,学习了
86
学习了
75
学习
77