Stroke:卒中-心脏综合征:卒中后心脏并发症的发生率和临床结局
2022-04-01 MedSci原创 MedSci原创
缺血性卒中后新发心血管并发症非常常见,主要不良心血管事件的5年预后明显较差。卒中及新诊断心血管并发症患者5年卒中复发发生率为50%。
卒中后主要不良心血管事件的风险显著增加。虽然以运动为基础的心脏康复已经被证明可以改善患者心脏事件后的预后,但它并不是卒中患者常规治疗的一部分。卒中后,个人患新发心血管并发症的风险增加。然而,卒中后新近诊断的心血管并发症的发生率和长期临床结局尚不清楚。近日,心血管疾病领域权威杂志Stroke上发表了一篇研究文章,研究人员旨在调查卒中患者心脏康复和主要不良心血管事件之间的关系。

这项回顾性队列研究使用了来自53个参与医疗保健组织的匿名电子病历。年龄≥18岁,随访5年的缺血性脑卒中患者被纳入研究。在缺血性卒中发生的4周内(暴露期)诊断为新发心血管并发症(心衰、严重室性心律失常、房颤、缺血性心脏病、Takotsubo综合征)的患者,倾向评分1:1匹配(年龄、性别、种族、共病、心血管护理)与未诊断为新发心血管并发症的缺血性卒中患者(对照组)。Logistic回归模型对5年全因死亡率、复发性卒中、住院和急性心肌梗死的发生率得到了比值比(OR)和95%CI。
研究人员对365383例的脑卒中患者进行5年随访;在发生缺血性卒中的4周内11.1%发生急性冠脉综合征;8.8%发生房颤/房扑;6.4%为心力衰竭;1.2%为严重室性心律失常;0.1%为Takotsubo综合征。倾向评分匹配后,与匹配的对照组相比,急性冠脉综合征卒中患者5年全因死亡率的比值显著升高(比值比为1.49[95%CI为1.44-1.54]),房颤/房扑(1.45[1.40-1.50]),心力衰竭(1.83[1.76-1.91]),严重室性心律失常(2.08[1.90-2.29])。
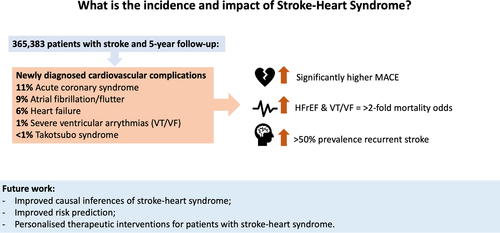
新发心血管并发症的卒中患者5年再住院和急性心肌梗死的几率也显著升高。Takotsubo综合征与5年复合主要不良心血管事件的发生率显著增高相关(1.89[1.29-2.77])。房颤/房扑是唯一一种新发心脏并发症,5年内缺血性卒中复发的几率显著增高(1.10[1.07-1.14])。
由此可见,缺血性卒中后新发心血管并发症非常常见,主要不良心血管事件的5年预后明显较差。卒中及新诊断心血管并发症患者5年卒中复发发生率为50%。
原始出处:
Benjamin J.R. Buckley.et al.Stroke-Heart Syndrome: Incidence and Clinical Outcomes of Cardiac Complications Following Stroke.stroke.2022.https://www.ahajournals.org/doi/10.1161/STROKEAHA.121.037316
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#并发#
68
#发生率#
47
#卒中后#
40
#临床结局#
0
#综合征#
28
学习了
37
学习了
40