赵志青:颈动脉狭窄支架术后再狭窄的原因分析及处理
2020-12-30 《门诊》杂志 门诊新视野
颈动脉术后再狭窄目前还未有最佳治疗方式,需要根据经验以及个体差异制定治疗方案。目前,CEA是CAS术后再狭窄的首选治疗方案。DCB联合CAS、DES可能会是未来颈动脉术后再狭窄腔内治疗的趋势。
颈动脉狭窄支架植入在临床应用广泛,但术后再狭窄问题不容忽视。2020年11月27日,第三届东方血管外科大会暨2020上海市医师协会血管外科医师分会年会期间,来自海军军医大学第一附属医院(上海长海医院)血管外科赵志青教授就颈动脉狭窄支架植入术后再发狭窄的原因及处理方式进行了详尽的解答。
颈动脉支架术后再狭窄发生率
World Neurosurg杂志上的一项荟萃分析研究表明:当以再狭窄度>70%为标准时,CAS术后再狭窄发生率为7.39%;当以再狭窄度>50%为标准时,CAS术后再狭窄发生率为18.21%。
ICSS研究表明:再狭窄度>50%时,术后1年的再狭窄度为27.8%,5年的再狭窄度为40.7%;再狭窄度>70%时,术后1年的再狭窄度为6.9%,5年的再狭窄度为10.6%.。可见颈动脉狭窄支架植入术后再狭窄的发生率相当高。
颈动脉支架术后再狭窄原因分析
1、早期再狭窄:血栓形成或机械性狭窄支架展开不全、支架远端流出道不佳、血栓形成、血管壁弹性回缩。
2、中远期再狭窄:内膜增生或血管负性重塑严重钙化、内皮损失、预扩张不充分、支架选择不佳、植入多枚支架、内膜增生或动脉硬化进展。
3、其它再狭窄原因斑块特征(如:斑块长度)、患者全身炎症状态、术后药物治疗依从性、年龄。有研究发现,CAS术后再狭窄更易发生于年龄较小的患者,这可能与年轻患者内膜增生能力更强,速度更快有关。
颈动脉支架术后再狭窄危险因素
World Neurosurg杂志上的这篇荟萃分析,还写到糖尿病、高血压病、高血脂症、女性、吸烟、肾功能不全、初发狭窄度>70%与颈动脉支架术后再狭窄的发生正相关。
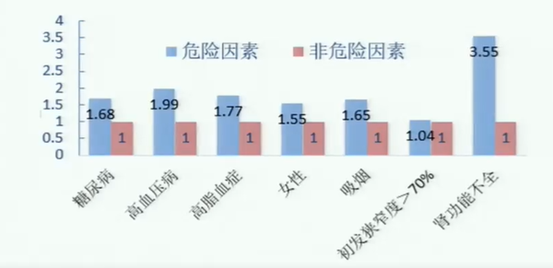
图1. 危险因素风险比
亚组分析表明:女性和吸烟与CEA术后再狭窄的发生密切相关;高血压病与CAS术后再狭窄的发生密切相关;CEA中采用补片修补的患者、症状性颈动脉狭窄运用CAS的患者与术后再狭窄的发生负相关。
颈动脉支架术后再狭窄分型(Mehran分型)
局限型:狭窄位于支架内或边缘部,狭窄长度≤10 mm;
弥漫型:狭窄处于支架内,狭窄长度>10 mm;
增生型:狭窄长度>10 mm,且狭窄扩展到支架外;
闭塞型:支架完全闭塞。
颈动脉支架术后再狭窄的处理
1、普通球囊PTA:
文献报道目前使用最常见的治疗方法,再发狭窄率高,持久性低。
2、切割球囊PTA:
2005年之后开始使用,具有一定效果。
3、载药球囊PTA:
抑制内膜增生,适合广泛弥漫的增生型再狭窄,不适合用于支架边缘的局限型再狭窄,容易引起夹层,需要普通球囊预扩张。
颈动脉术后再狭窄的药涂球囊治疗:目前有几项前瞻性研究报道,药涂球囊在颈动脉术后再狭窄的预防及治疗上有良好的短、中、长期效果;而研究的证据等级不足在于样本量都偏小,选择偏倚大。
4、CAS:
PTA and repeat CAS:能够降低再发再狭窄的风险,但是再次植入支架并不增加绝对管腔,还更易引起内膜增生,远期再次发生狭窄风险高。
DCB联合CAS:DCB扩张颈动脉再行CAS能降低再发狭窄的风险。载药支架(DES):正在兴起,偶有报道,缺少大样本数据支持。
5、CEA with stent removal:
目前较为安全有效的方法。手术难点在于:CAS术后刺激动脉周围炎症反应,影响血管暴露;支架与血管内膜黏连紧密,导致剥离支架困难;支架过长导致阻断血流困难。
颈动脉支架术后再狭窄的预防
1、药物预防
抗血小板药:抑制内膜增生和血小板活化的作用。有文献报道,阿司匹林联合氯吡格雷、西洛他唑能更好的降低颈动脉再狭窄发生率;
他汀类药物:降脂、稳定斑块,抑制平滑肌迁移;
胰岛素:控制血糖,抑制平滑肌迁移;
缬沙坦:控制血压,抑制血管紧张素受体进而降低再狭窄发生率。
2、影像学随访
颈动脉超声为CAS术后随访的首选检查;
CDU在诊断CAS术后再狭窄程度中具有更高价值。
小 结
颈动脉术后再狭窄目前还未有最佳治疗方式,需要根据经验以及个体差异制定治疗方案。目前,CEA是CAS术后再狭窄的首选治疗方案。DCB联合CAS、DES可能会是未来颈动脉术后再狭窄腔内治疗的趋势。当然,颈动脉狭窄术后再狭窄防胜于治,并遵循个体化治疗。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#支架术#
44
#支架术后#
41
#颈动脉#
52
#再狭窄#
0
#动脉狭窄#
47