IgG4相关性慢性硬化性脑膜炎1例
2019-02-01 阳吉虎 纪涛 郭见 中国临床神经外科杂志
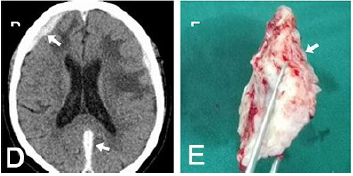
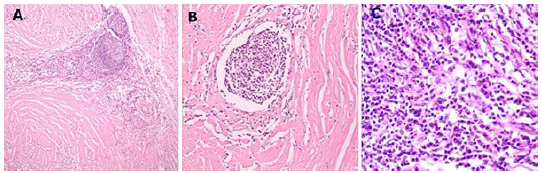
男,53岁,因双下肢活动障碍4年、加重10 d入院。4年前,头颅MRI示双额颞硬膜下血肿(图1A、1B),MRV示矢状窦闭塞(图1C),保守治疗好转出院,之后反复出现癫痫发作,双下肢活动障碍。10 d 前,双下肢活动障碍加剧,不能站立。体格检查:双上肢肌力、肌张力正常,双下肢肌力3级,肌张力呈齿轮样强直,双侧Babinshi征(+),Kerning征(-)。


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#相关性#
34
#IgG4#
28
#硬化性#
43
#IgG#
28