Dig Liver Dis: 新蝶呤水平升高与肝硬化患者的慢性肝功能衰竭和死亡率相关
2020-08-13 MedSci原创 MedSci原创
巨噬细胞活化在肝脏和全身性炎症中起着核心作用,并参与了急慢性肝衰竭(ACLF)的发病机理。
巨噬细胞活化在肝脏和全身性炎症中起着核心作用,并参与了急慢性肝衰竭(ACLF)的发病机理。那么有一种生物标志物——新蝶呤,它的水平反映了整体巨噬细胞的活性,它在传染性,心血管性,神经变性,自身免疫性疾病中都会明显升高。因此,本研究旨在调查肝硬化急性失代偿期(AD)患者的新蝶呤水平,评估其与ACLF和预后的关系。

本项研究为前瞻性队列研究,研究人员将205名因肝硬化急性失代偿(AD)住院的成年受试者纳入研究。将21名健康受试者和89名稳定肝硬化患者作为对照。与稳定的肝硬化和健康对照相比,AD中新蝶呤的含量更高( p <0.001)。ACLF与新蝶呤水平较高独立相关(OR 1.015,95%CI 1.002-1.028, p = 0.025)。在多元Cox回归分析中,新蝶呤水平(HR = 1.002,IC 95%1.000–1.004, p = 0.041),Child–Pugh C级和ACLF是30天生存率的预测指标。在ACLF患者中,新蝶呤水平<25 nmol / L的患者的Kaplan–Meier生存概率为71.4%,如果新蝶呤≥25 nmol / L的患者的Kaplan–Meier生存率为31.0%( p <0.001)。

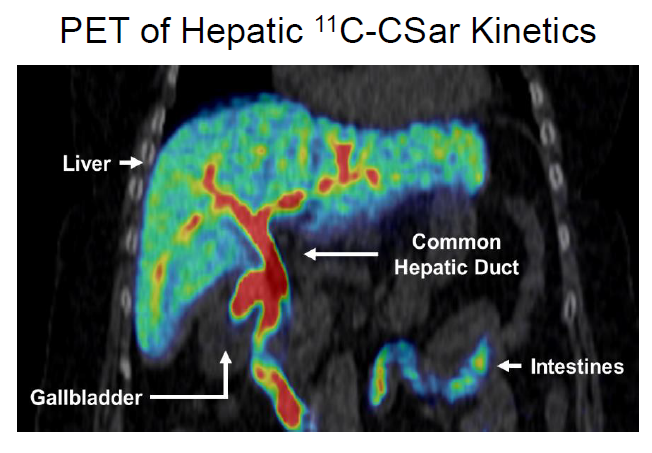
图:肝硬化急性失代偿患者新喋呤水平明显升高
因此,作者最后说道:肝硬化AD住院的患者中,较高的循环新蝶呤与ACLF相关。新蝶呤水平也是短期死亡率高的独立预测因素。
原始出处:
Camila Matiollo. Et al. Elevated neopterin levels are associated with acute-on-chronic liver failure and mortality in patients with liver cirrhosis. Dig Liver Dis.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#新蝶呤#
40
#Dis#
36
#肝功能衰竭#
68
#肝功能#
40
谢谢!最新的信息读起来就是收获大
66