JAMA Cardiol:女性冠心病发病年龄与血脂、炎症和代谢生物标志物的相关性
2021-01-22 MedSci原创 MedSci原创
包括冠心病(CHD)在内的心血管疾病是导致过早死亡(英年早逝)的一个重要因素。早发性冠心病通常是指女性65岁之前或男性55岁之前发生的CHD。目前早发性CHD的风险特征尚不清楚。
包括冠心病(CHD)在内的心血管疾病是导致过早死亡(英年早逝)的一个重要因素。早发性冠心病通常是指女性65岁之前或男性55岁之前发生的CHD。目前早发性CHD的风险特征尚不清楚。
该研究旨在调查女性冠心病发病年龄时的基线风险分布。研究人员对参与妇女健康研究的美国女性健康专业人员进行了前瞻性队列研究;平均随访时间为21.4年。共28?024名45岁或以上且无已知心血管疾病的女性。收集了1993年4月30日-1996年1月24日的基线概况,并在2017年10月1日-2020年10月1日进行了分析。
评估指标有超过50种临床、脂质、炎症和代谢危险因素和生物标志物。主要预后为CHD的发病年龄(<55岁、55岁~65岁、65岁~75岁和≥75岁)。
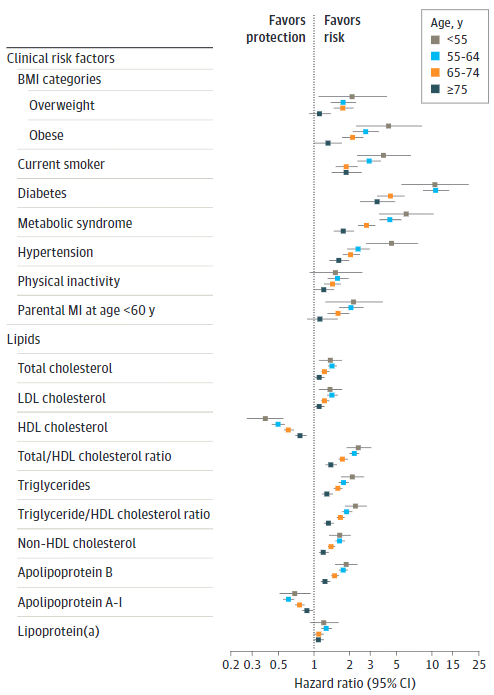
临床风险因素和脂质生物标志物与不同年龄段发生CHD的相关性
在女性的临床因素中,糖尿病对冠心病发病的校对风险比(aHR)最高,从55岁以下发病者的10.71(95%CI 5.57-20.60)到75岁以上者的3.47(2.47-4.87)。55岁以下参与者发生冠心病的风险因素还包括代谢综合征(aHR,6.09;95%CI 3.60-10.29)、高血压(4.58;2.76-7.60)、肥胖(4.33;2.31-8.11)和吸烟(3.92;2.32-6.63)。父母在60岁之前发生心肌梗死与75岁以下个体患冠心病的风险升高1.5-2倍有关。在大约50个生物标记物中,脂蛋白胰岛素抵抗在55岁以下女性发生冠心病的标准化aHR值最高:6.4(95%CI 3.14-13.06),该相关性随着年龄的增长而减弱。
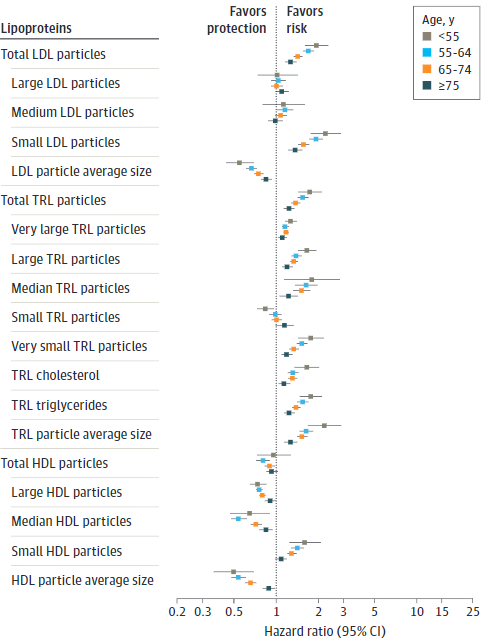
不同脂质指标与不同年龄段发生CHD的相关性
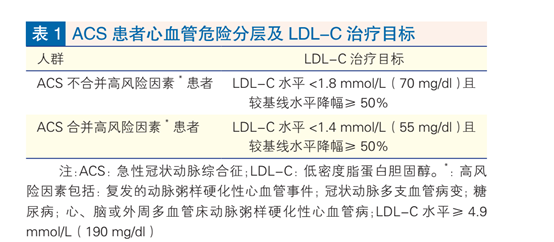
相比之下,在55岁以下女性中,低密度脂蛋白胆固醇(aHR 1.38;95%CI,1.10-1.74)、非高密度脂蛋白胆固醇(1.67;1.36-2.04)、载脂蛋白B(1.89;1.52-2.35)、甘油三酯(2.14;1.72-2.67)和炎性生物标志物(1.89;1.52-2.35)与冠心病的相关性较弱但显著--都随着年龄的增长而减弱。
炎症指标与不同年龄段发生CHD的相关性
部分生物标记物具有相似的冠心病年龄相关性(如,缺乏运动、脂蛋白[a]、总高密度脂蛋白颗粒),而少数生物标志物与任何年龄的冠心病发病都无关。大多数风险因素和生物标志物与冠心病发生的相关性都随着年龄的增长而减弱。
综上,在这项队列研究中,除了高血压、肥胖和吸烟外,糖尿病和胰岛素抵抗似乎也是早发性冠心病的最大危险因素。大多数风险因素的贡献在老年人中都相对降低了。
原始出处:
Sagar B. Dugani, et al. Association of Lipid, Inflammatory, and Metabolic Biomarkers With Age at Onset for Incident Coronary Heart Disease in Women. JAMA Cardiol. January 20, 2021. doi:10.1001/jamacardio.2020.7073
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Cardiol#
38
#相关性#
28
#标志物#
41
#生物标志#
39
#生物标志#
36
#发病年龄#
35
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
49