Front Oncol:外科医师对微创手术的熟练程度影响早期宫颈癌患者的预后:来自851例患者的回顾性研究
2021-11-17 yd2015 MedSci原创
研究表明,外科医师微创手术(MIS)的熟练程度可影响早期宫颈癌患者的预后,随着手术病例的增多,可逐渐达到良好预后。
近期,Frontiers in Oncology杂志上发表了四川大学研究团队的一项研究成果,比较早期宫颈癌患者接受外科微创手术(MIS)的临床疗效,以及评估外科医生的熟练程度是否影响生存。
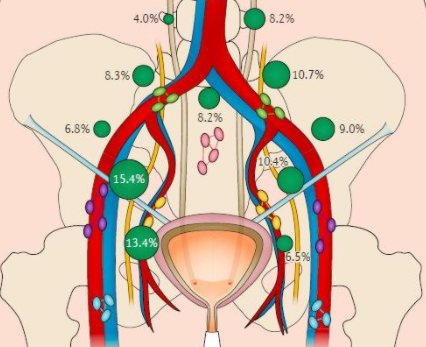
回顾性分析2008年1月至2018年6月(每年1月至6月)行根治性子宫切除术(RH)的851例早期宫颈癌患者。根据外科医师微创手术的熟练程度将患者分为4个阶段(第一阶段,1-10例;第二阶段:11-20例;第三阶段:21-30例;第四阶段:>30例)。收集并分析人口统计资料、临床和病理资料。
研究共纳入851例患者:开放手术组510例,MIS组341例(无机器人RH)。患者平均年龄46.51岁(范围18-73岁;标准偏差[SD] 9.33),大部分患者(471例,55.35%)诊断为IB1期。开放手术组与MIS组在年龄、绝经期、BMI、组织学亚型和分级方面无显著差异。开放手术组以晚期FIGO分期及宫颈深层间质浸润多见。开放手术组的中位住院时间为8天(范围3-30),MIS组的中位住院时间为7天(范围3-21)(p<0.001)。开放手术组中位手术时间为200分钟(85-510),MIS组中位手术时间为240分钟(75-450)(P<0.001),开放手术组中位失血量为400 mL(范围50-2500 mL), MIS组中位失血量为200 mL(范围10-4500 mL) (P<0.001)。
开放手术组和MIS组的中位随访时间分别为88.6个月和62.2个月。3年、5年OS和DFS的差异无统计学意义(3年OS: 94.5% vs. 96.4%;5年OS: 93.4% vs. 96.0%;P = 0.291; 3年DFS: 94.4% vs 94.6%,5年DFS: 92.8% vs 94.2%,P = 0.585)。在调整了年龄、BMI、FIGO分期、组织学亚型和分级后,使用多变量Cox比例风险回归模型获得了相同的结果[OS: P = 0.894, HR 1.039, 95%CI (0.593, 1.820);DFS, p = 0.647;HR,0.891;95% CI(0.544, 1.460))。此外,研究还分析了开放手术组和MIS组各位手术医师治疗对生存影响,发现生存仍无统计学意义(所有p值>0.05)。
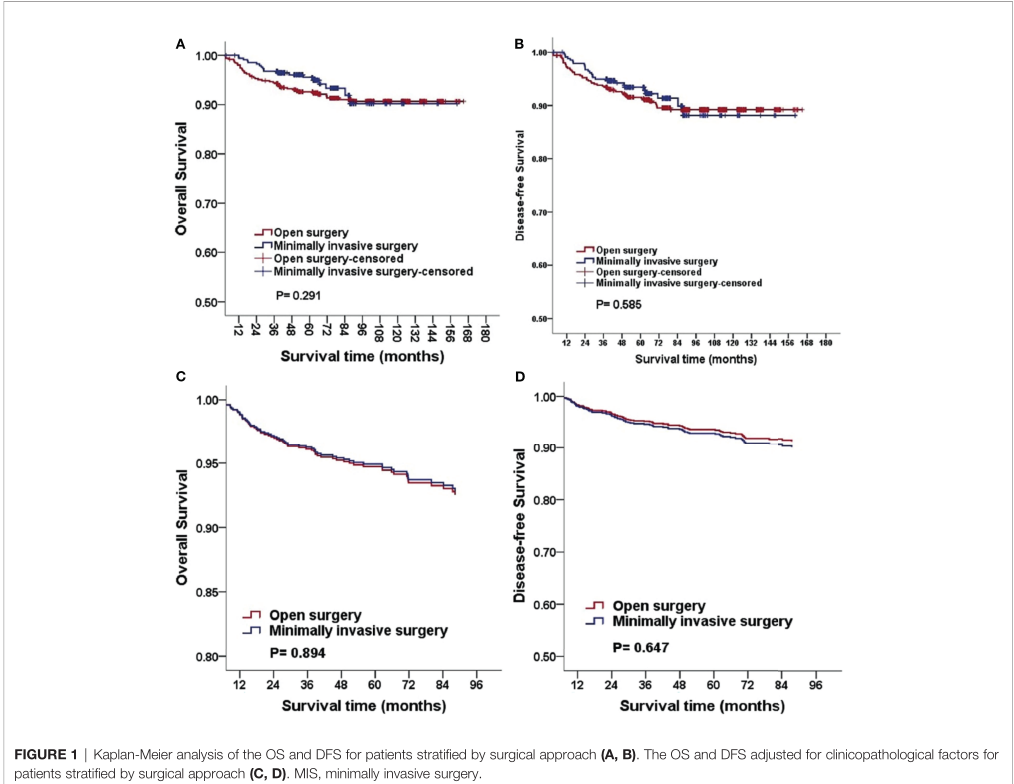
开放手术和微创术后对预后影响
对于每一位外科医生,根据外科医师微创手术的熟练程度将患者分为4个阶段(第一阶段,1-10例;第二阶段:11-20例;第三阶段:21-30例;第四阶段:>30例)。考虑到开放手术是比较成熟技术,研究没有对该组患者进行不同阶段的分类。按不同阶段分层时,经年龄、BMI、FIGO分期、组织学亚型、分级等因素调整后,MIS组第一阶段手术的OS和DFS明显低于后期和开放手术组。MIS组第一阶段手术患者3年OS为91.8%(45/49),5年OS为87.8% (43/49)(P = 0.009; HR,2.896; 95%CI,1.303-6.435)。MIS组第一阶段手术患者3年DFS为91.8%(45/49),5年DFS为85.7% (42/49)(P = 0.009; HR,2.712; 95%CI,1.289--5.706)。当单独分析外科医生时,得到了相似的结果。
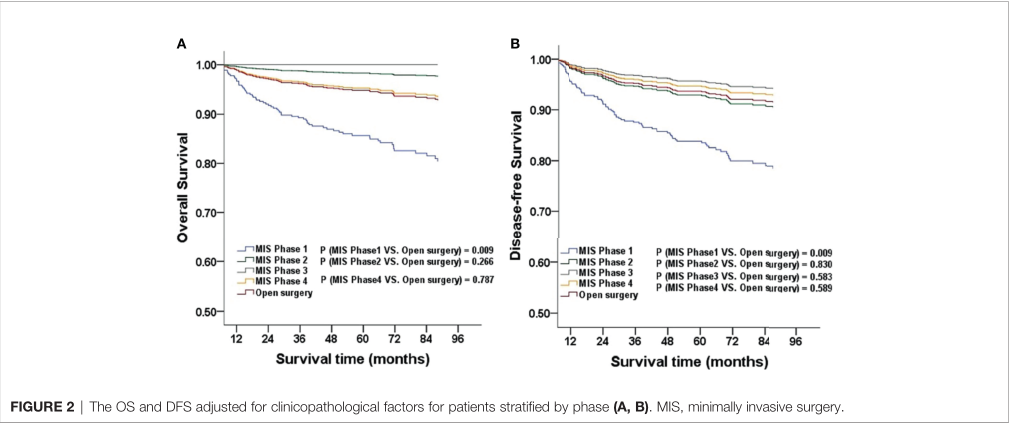
术者不同阶段微创手术对预后影响
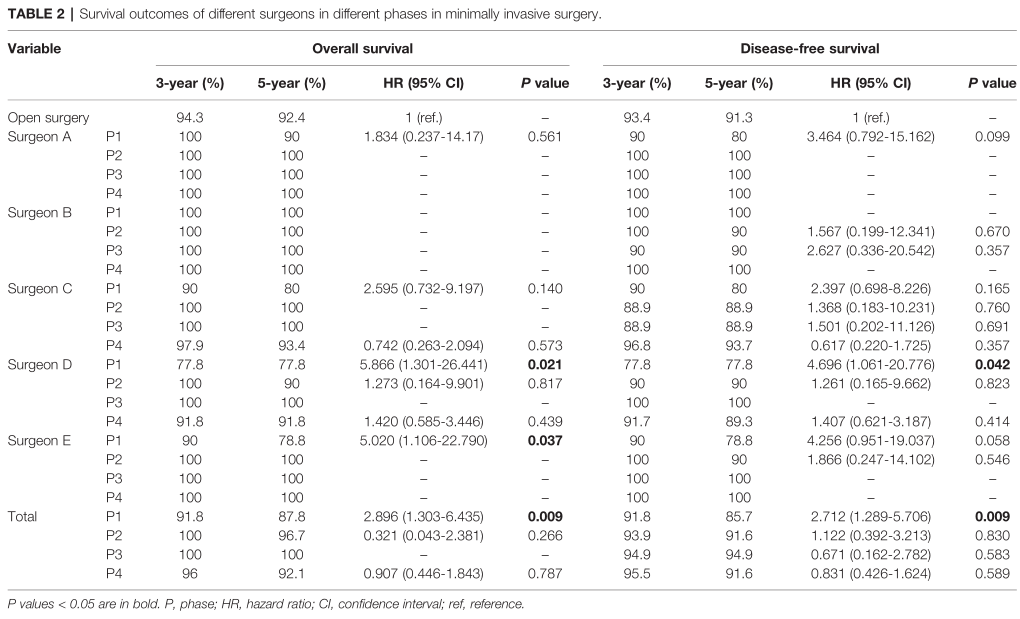
不同术者不同阶段对预后影响
对不同术者进行比较,调整后生存率无统计学意义。进一步的相应阶段的亚组分析结果一致(P >0.05)。
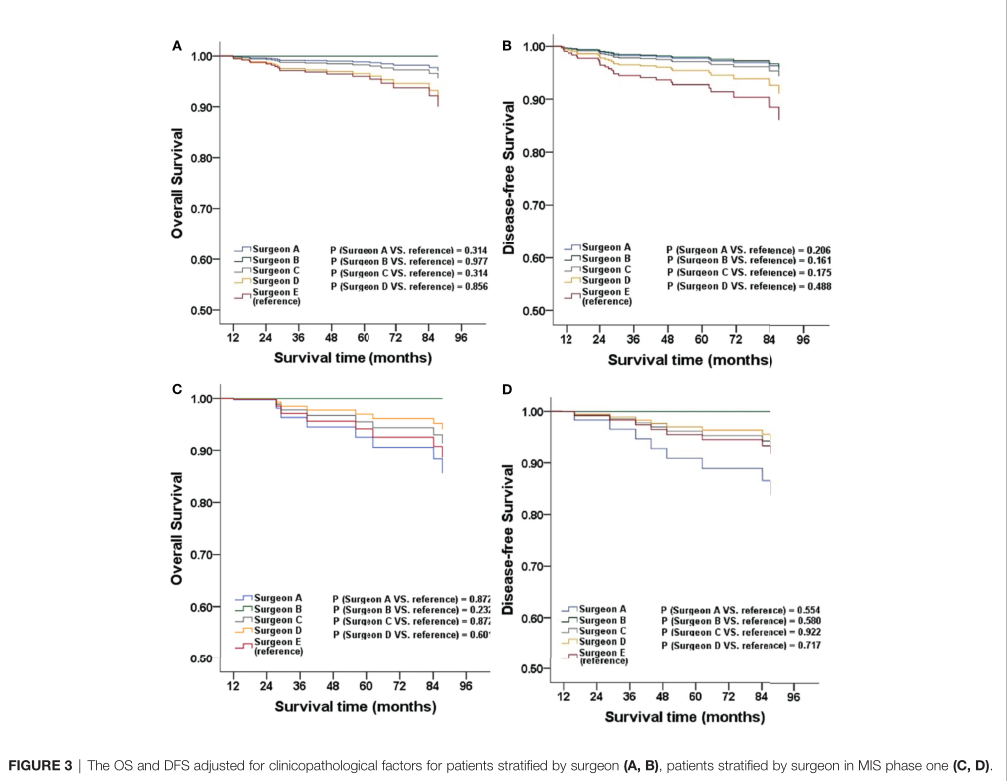
不同术者对预后影响
综上,研究表明,外科医师微创手术(MIS)的熟练程度可影响早期宫颈癌患者的预后,随着手术病例的增多,可逐渐达到良好预后。
原始出处:
Yang Y, Huang Y and Li Z (2021) The Surgeon’s Proficiency Affected Survival Outcomes of Minimally Invasive Surgery for Early-Stage Cervical Cancer: A Retrospective Study of 851 Patients. Front. Oncol. 11:787198. doi: 10.3389/fonc.2021.787198
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#Oncol#
26
#微创手术#
39
#微创#
32
#宫颈#
30
#回顾性研究#
41
我去思路清奇
42
学习了,谢谢分享
38